Case study
12 Jun: How a Multi-Hospital, Multi-Specialty Physician Practice Eli...
While physician practices commonly struggle to collect revenue for all the services they provide, one multi-hospital, multi-specia ...
Blog
05 Jun: Revolutionize your Revenue Cycle and Clinician Workflow with...
Ingenious Med’s New AI-powered automated charge capture solution delivers the power of AI and automation directly to your provid ...

Blog
21 Apr: 2025 MGMA Focus | Financial Conference: Top 3 Takeaways
At this year’s MGMA Focus | Financial Conference, we encountered a strong sense of exuberance that today’s financial leaders ...

Blog
19 Feb: 5 Ways Independent Physician Practices Can Generate More Rev...
Independent physician practices are continuing to dwindle in numbers. Nearly 80% of all physicians were affiliated with hospitals, ...

Blog
24 Jan: Next-Gen RCM Expectations for 2025: AI Driving Double-Digit ...
Heading into the New Year, healthcare provider organizations are now actively investing in AI to address persistent revenue cycle ...
Blog
07 Jan: Ingenious Med® Successfully Earns Renewal of SOC 2 Report t...
At Ingenious Med, we continually invest in security best practices to ensure that our client’s data stays safe and secure. As a ...

Blog
09 Dec: Reliability Science: Optimizing Revenue with Charge Note Rec...
Is your revenue cycle ‘highly-reliable’ to the point that your physician practice is capturing 100% of the charges you should? ...
Blog
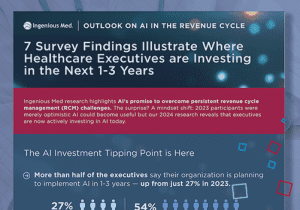
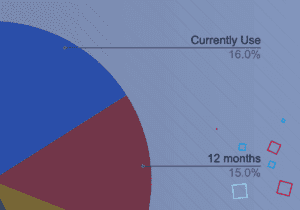
02 Dec: Research Signals Investment Plans for AI in Revenue Cycles A...
Ingenious Med commissioned an independent survey of 101 finance and operations leaders to understand executives’ expectations ab ...
Blog
11 Nov: Driving Revenue Cycle Success for TeamHealth with Ingenious ...
Almost every hospital, health system, and medical group struggles to maximize revenue cycle management and overall financial perfo ...
Blog
24 Oct: The New Charge Capture Conundrum: EMR-Embedded Tools Lead to...
With healthcare costs projected to rise another 8% year-over-year in 2025, and research showing that providers delivered $745 bill ...

White papers
07 Aug: Market Report 2024 – From AI Optimism to Action
From AI Optimism to Action: Where Health Systems, Hospitals, and Practices are Investing Now to Fortify Revenue Cycle Management
...
Blog
22 Jul: A Solution for Lagging Physician Productivity: Analytics, Co...
New research commissioned by Ingenious Med finds that 75% of healthcare leaders do not have adequate insight into physician produc ...

Blog
03 Jun: The Untapped Power of Revenue Cycle Management Tools: Care T...
New Ingenious Med-funded research shows that 86% of hospitals and health systems still rely, at least in part, on their electronic ...

Blog
29 Apr: Too many EHRs Hurting Your Revenue Cycle? Time To Look Elsew...
Ingenious Med funded research that reveals healthcare leaders believe AI holds powerful potential to optimize revenue cycles.
82% ...
Case study
22 Mar: Redesigning Physician Productivity to Address Workforce Shor...
Hospitals have been struggling with labor productivity for years1 and hospitalists specifically have seen very little increase in ...
Blog
11 Mar: Ransomware in the Revenue Cycle: Protecting Your Ability to ...
Cyberattacks can block hospitals and health systems from filing claims or collecting revenue.
Here are three ways to safeguard a ...

Blog
05 Feb: 7 Revenue Cycle Management Trends for 2024
Hospital revenue cycles, and the professionals who manage them, are under immense pressure heading into 2024. Early last year, Fit ...
Blog
15 Jan: The Urgent AI Opportunity in Revenue Cycle Management: Creat...
Today’s revenue cycles are at a crossroads: hospital and health system leaders are not particularly satisfied with their revenue ...

Blog
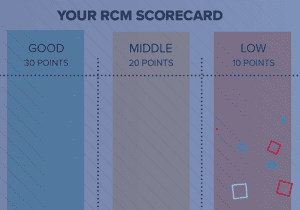
29 Nov: The RCM Scorecard: How Well Is Your Healthcare Organization ...
Top 10 Revenue Cycle Management metrics hospitals and physician groups should master
Amid rising costs of care delivery, work ...
Blog
27 Nov: The Ingenious Med Revenue Cycle Management (RCM) Scorecard
Amid rising costs of care delivery, workforce shortages, and reimbursement challenges, it’s more important than ever for hospita ...

Blog
06 Nov: HITRUST Certification: What it Means to Our Customers and to...
Ingenious Med is certified by the HITRUST Alliance for data protection and risk management to safeguard sensitive health informati ...
White papers
24 Oct: 5 Steps to Improving Financial Performance for ASCs
Ambulatory surgery centers are at a unique intersection: rising patient volumes are contributing to increased revenue, but managin ...
Blog
25 Sep: RCM best practices and the potential for AI assistance
This article was featured in Physician's Practice
Healthcare providers have long struggled to get paid for ...
Blog
31 Aug: MIPS 2024: Inpatient Practices Must Advocate for Equitable S...
MIPS Challenges for Inpatient Clinicians in 2024
Quality will continue to be the most influential category in the MIPS scoring pr ...
Blog
31 Jul: Unleashing the Power of MIPS: Benefits, Consequences, and Fi...
In today's rapidly evolving healthcare landscape, the Merit-Based Incentive Payment System (MIPS) has emerged as a transformative ...

White papers
21 Jul: Where Does it Hurt? The Many Sources of Pain in RCM and the ...
Primary research sponsored by Ingenious Med, a leading physician productivity and hospital performance solution, found that health ...
Blog
04 May: Preventing Rising Claims Denials
3 Ways a Point-of-Care Charge Capture Solution Can Help Reduce Rising Claims Denials
Despite advances in technology and automatio ...

Blog
04 Apr: Five Ways Independent Physician Practices Can Generate More ...
As a growing number of physicians become employed in practices owned by health systems or investors, these independent physician o ...

Blog
06 Mar: Continuous Improvement of Revenue Capture Integrity: Ingenio...
Ingenious Med is Approved and Available at Both Cerner CODE and Epic App Orchard
Recognizing the industry need for secure system ...

Blog
20 Jan: Preventing Cyber Attacks: 4 Steps Your Vendor (and Your Heal...
How to go beyond check-the-boxes approaches to strengthen vendor security
Cybersecurity has become a top concern for healthcare ...

Blog
05 Dec: Out of the Frying Pan: From Pandemic to Inflation
The financial challenges of running a health system, hospital or healthcare practice never seem to abate. Instead of getting a bre ...

White papers
01 Nov: How to Help Your CFO Sleep Better at Night
As the fallout from the pandemic lingers, healthcare organizations are seeing expenses rise faster than patient volumes or revenue ...

Blog
31 Oct: CFO’s Guide to a Restful Night’s Sleep
Need more restful sleep? Here are five steps to better financial health for healthcare CFOs and other financial leaders. ...

Blog
30 Aug: From Minimizing Denials to Minimizing Risk: How to Move RCM ...
RCM Risk Management: 3 Ways Point of Care Tools Can Help Your Revenue Cycle Evolve
Most healthcare revenue today is tied in some ...

Blog
08 Jul: 3 Keys to Building a Strong Home-Based Care Program
How point of care tools can help stop the revolving door
Can an investment in post-acute care keep patients safe at home while ...

Blog
06 Jun: Three Ways to Address Coding and Billing Staff Challenges
Healthcare organizations have found it increasingly challenging to hire and retain qualified medical coders and billers in the pas ...

Blog
03 May: The Cure for the Many Disadvantages of Paper Consent Forms
And What to Look for in an eConsent Platform
While much of healthcare has been digitized, surgical and other patient consent fo ...

Blog
29 Mar: Strategies and Tools to Revitalize Value Based Care in Your ...
Value-based care (VBC) took a backseat during COVID but is poised to be re-energized, according to presenters at our recent webina ...

Blog
04 Feb: Making Technology More Accessible for All at Ingenious Med
The Americans with Disability Act (ADA) was passed in 1990 to ensure that those with visual, ambulatory, or other disabilities wer ...

Blog
07 Jan: Whether you Insource or Outsource, How to Collect More with ...
Which is better, outsourcing or insourcing your billing? As is often the case, the answer is, ‘It depends on your practice.’ W ...

Blog
29 Oct: 6 Tips for Hospitalists and Healthcare Organizations to Join...
In the past decade, hospitalist subsidies more than doubled and their compensation increased about 40%. Those were just two of the ...

Blog
21 Oct: MIPS Extreme and Uncontrollable Circumstances Exceptions for...
The good, the bad, and the ugly — and how to avoid penalties
As COVID-19 continues to disrupt normal operations for medical pra ...

White papers
07 Sep: Maximizing Margins with More Efficient RCM
This white paper shares how three leading healthcare organizations — AtlantiCare Regional Medical Center, Community Health Syste ...

Blog
14 Jul: 5 Steps to Greater Financial Efficiency: Customers Share Wha...
Ingenious Med sponsored a webinar with RevCycleIntelligence in late May in which two of our clients shared five ways they optimize ...

Blog
07 Jul: How to take on more risk without risking your practice (Valu...
By Steve Liu, MD
The arrival of COVID in the early part of 2020 caused the volume of non-infected patients to plummet and force ...

Blog
27 Apr: Five Ways Independent Physicians Can Capture and Keep More R...
The healthcare industry has often predicted that independent physicians will become an endangered species, and there’s no questi ...

Blog
15 Apr: Ingenious Med: Supporting a Comprehensive Productivity Optim...
TeamHealth, one of the nation’s leading integrated physician practices with almost 16,000 clinicians in various specialties that ...

White papers
22 Mar: How to Minimize Physician Burnout and Optimize Revenues: Les...
Physician burnout was rampant prior to COVID-19, but as the pandemic wears on, it has heightened existing financial, physical, and ...

Blog
15 Feb: Six Strategies for Preventing Administrative Burnout
Even before the pandemic struck in early 2020, healthcare coding and billing staff were experiencing burnout due to staffing short ...

Blog
04 Jan: 2020 MIPS Relief for Extreme and Uncontrollable Circumstance...
By Stephen Besch, Director of Clinical Quality Reporting
Between rising COVID cases, falling elective procedure volum ...

Blog
01 Dec: 3 Ways Data Reduces Physician Burnout and Enhances Revenues ...
Burnout.
It was rampant among healthcare providers even before COVID-19. According to two recent surveys, the virus is now rais ...

Blog
04 Nov: Five Revenue Cycle Optimization Tactics for the COVID Surge
Even before COVID-19 hit, hospitals were struggling to make ends meet with nearly a third operating at a loss. ...

Blog
23 Oct: The Case for Prioritizing Revenue Cycle Optimization
Delivering high-quality patient care is the primary goal for physicians. But declining reimbursements and tighter margins mean tha ...

Blog
22 Oct: Medical Billing Experts: Key to Your Organization’s Financ...
Even before COVID-19 turned the economics of healthcare upside down, managing the business side of health systems and physician gr ...

Blog
13 Oct: Four Benefits of Automating Charge Note Reconciliation
Technology has long promised to ease administrative burdens on physicians and healthcare staff, but has a poor track record of del ...

White papers
12 Oct: Rising to the Challenge: How Leading Healthcare Organization...
Operating health systems and physician practices has always been hard, but COVID-19 has created extraordinary profitability challe ...

Blog
11 Sep: Proactively Improve Your Charge Capture with Internal Auditi...
If you do not have an internal charge capture audit program, you could be leaving money on the table or inviting an external audit ...

Blog
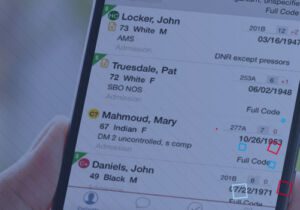
09 Sep: 5 Functions that Improve Practice Management and Back-Office...
Thousands of healthcare systems, hospitals and physician practices rely on the Ingenious Med® application to capture charges and ...

Blog
26 Aug: How to Harness the Power of Data to Improve Physician Produc...
Physicians and the care they provide patients are at the heart of any healthcare organization. If they are not meeting performance ...
Blog
19 Aug: New Survey Shows Telehealth Growth
Providers face a fragmented market, lack EHR integration and need better charge capture
After hearing from many customers and rea ...

Blog
13 Aug: 5 Questions to Ask about Revenue Cycle Analytics
Many healthcare organizations overlook untapped resources that can improve the revenue cycle management process, which depends on ...

Blog
13 Aug: Mastering Medical Coding Compliance
Merely mentioning coding compliance to a physician may produce responses ranging from an eyeroll to dread and anxiety. The entire ...

Blog
14 Jul: 5 Ways to Increase Revenue with Healthcare Business Analytic...
Healthcare organizations have experienced drastic volume declines in 2020 as well as the stress of caring for an unprecedented num ...
Blog
06 Jul: Care Coordination and Care Collaboration: Improving Clinical...
Successfully aligning physician performance with the Triple Aim goals of reducing per capita healthcare costs, increasing care qua ...

Blog
26 Jun: Seven Ways to Turbocharge Your Practice with Physician Tools
Electronic Health Records (EHR) are vital for the daily operations of a medical practice, but they are only one part of the IT too ...

Blog
12 Jun: COVID-19 as a Catalyst for Change
How health systems can optimize revenues and resources
By Nimesh Shah, CEO, and Laura Chapman, VP of Product Management
The C ...

Blog
10 Jun: The App Gap: 6 Essential Capabilities Your EHR Apps May Miss
Electronic health records cannot cover every clinical and operational hospital function, and the mobile versions of these systems ...

Blog
05 Jun: MIPS Registry and Reporting: Increase Quality Time with Pati...
MACRA, MIPS, APM… the alphabet soup of medical documentation and billing can be daunting. Providers trained to improve health fi ...

Blog
02 Jun: Mobile Charge Capture: The Key to Practice Revenue Optimizat...
Mobile charge capture might not be the first thing on the minds of healthcare providers as they focus on the health and well-being ...

Blog
12 May: Coping with COVID-19 – Part 2
How Front-Line Healthcare Leaders are Strategically Managing Resource Challenges During the COVID-19 Crisis
In April 2020, Ingeni ...
Blog
30 Apr: Coping with COVID-19 - Part 1
How Front-Line Healthcare Leaders are Solving Financial Challenges During the Covid-19 Crisis
On April 9, 2020, Ingenious Med CEO ...

Blog
01 Apr: Five ways to overcome revenue cycle disruption during the CO...
Rising costs. Canceled surgeries and routine visits. Uncertain reimbursements for COVID-19 patient care. Longer lengths of stay in ...

Blog
17 Mar: What’s holding us back from accurately evaluating performa...
In value-based care programs, flying blind is ill-advised. As more value-based care models incorporate two-sided risk, healthcare ...

White papers
05 Mar: From Data Lakes to Insight Streams: Connecting clinicians to...
Healthcare organizations collect massive amounts of clinical, financial and operational data. But they’re often challenged by th ...

Blog
10 Feb: Point-of-care charge capture: Why it’s better for revenue ...
With intensifying pressures to grow revenues while managing costs, health systems and physician practices are renewing their effor ...

Blog
16 Jan: 2020 Vision: The Top Five Trends Shaping Healthcare Tech
By Steve Liu, MD, Founder & CMO, and Jim Hall, Chief Revenue Officer
As we look ahead to a new decade and a year whose very ...

Blog
05 Dec: Facility-Based Scoring: Your 2019 MIPS Safety Net
By Stephen Besch, Director of Clinical Quality Reporting
After a few years of relative stability, changes are afoot once again ...

Blog
20 Nov: How health IT can improve coordination and quality while red...
By Robert Pearl, MD, guest blogger
The technology boom of the 1990s promised to give physicians access to comprehensive patient ...

Blog
07 Nov: Top Takeaways from Becker’s Hospital Review 2019 Health IT...
What your health system needs to know
By Laura Chapman, VP of Product Management and Kevin Nicholas, VP of Marketing
It’s al ...

Blog
24 Oct: Act now to avoid penalties as claims-based MIPS reporting en...
By Stephen Besch, Director of Clinical Quality Reporting
The rewards and risks of MIPS continue to grow, with a range of plus o ...
White papers
03 Oct: Overcoming blind spots: How analytics improve healthcare per...
Healthcare is changing rapidly. While margins shrink and care shifts beyond hospital walls, health systems must prove their value. ...
Blog
25 Sep: Aligning physicians and health systems through analytics
by Steven Liu, MD, SFHM, Founder and Chief Medical Officer
Our recent webinar, Overcoming Blind Spots: Using Analytics to Impro ...

Case study
20 Aug: Extending EHR value with Ingenious Med
EHR transitions are costly – and not only in terms of dollars. There is also the toll taken on your organization’s productivit ...

Blog
07 Aug: Extending the Value of your EHR: What does it take?
As hospitals go through the different stages of EHR adoption, they need different strategies. Having robust revenue capture tools ...

White papers
17 May: Driving a Better Bottom Line Through Intelligent Data
Hospitals and health systems are constantly challenged to grow revenues and reduce costs. At the same time, they must meet the dif ...
Case study
14 Mar: A Clearer View: Managing Data Within Health Systems
A Clearer View: Managing Data Within Health Systems
How one large health system uses the Ingenious Med platform to optimize reven ...

White papers
15 Jan: How Mobile Technology is Shaping the Future of Healthcare
As healthcare technologies continue to advance, mobile health — often referred to as “mHealth” — has emerged as a popular ...
Blog
02 Jan: Revenue Cycle Top Performers - Infographic
What makes a top performer different than the rest of the market? Here are 5 questions your organization should answer if you want ...

White papers
17 Dec: A Finely Tuned Machine - Six Financial Takeaways
Very little research has been done on the front end of the financial revenue cycle: professional fee charge capture. To fill this ...
Blog
13 Dec: How RCM top performers stay ahead of the curve
While healthcare organizations often take similar approaches to revenue cycle management, the financial top performers distinguish ...
Case study
11 Dec: High-Value Revenue Cycle Management: The Right Data at the R...
Despite the growing emphasis on data in healthcare, many organizations are struggling to acquire it. And even when they do have th ...
Blog
06 Dec: Five Ways Hospital Leaders Can Improve Charge Capture
There are some small steps healthcare executives can take to ensure their hospital is capturing the right charges — and not the ...
Case study
03 Dec: Harnessing the Power of Revenue Cycle Analytics
According to a recent market research study by Ingenious Med, only 1 in 3 healthcare executives currently believe they have enough ...

Blog
03 Dec: How Top Performing Health Organizations Reduce Missed Charge...
One of the most effective ways to improve a healthcare organization is to learn from other successful organizations. Healthcare le ...

Blog
16 Nov: Leveraging Data to Drive Better Value-based Decisions
These organizations possess a vast amount of clinical, operational, and financial data, but it is exceptionally difficult to proce ...

Blog
13 Nov: 4 Questions to Answer with Physician Performance Metrics
To identify areas where performance metrics could improve quality care and revenue cycle processes, ask the following questions of ...
Case study
09 Nov: Master Coding Efficiencies, Minimize Under- and Over-Coding
Every part of the revenue cycle is vital to an organization’s financial health, yet not every aspect is treated equally. The cod ...
Blog
23 Oct: Optimizing the Charge Capture Process - Infographic
In 2018, Ingenious Med commissioned a study to determine what differences and similarities existed between acute-care organization ...
Blog
22 Oct: Identifying Charge Capture Best Practices to Improve RCM
Though healthcare organizations consider revenue cycle management (RCM) one of the most important aspects of business, little rese ...
Case study
22 Aug: Adfinitas Case Study
SUMMARY
Organization: Adfinitas Health
Location: Hanover, Maryland
Size: 500 employees; 50 hospitals and post-acute facilitie ...
Blog
21 Aug: Health IT and Care Quality: An Efficient Partnership
Critics in the medical industry have historically shown a skeptical attitude toward the implementation of new technology in health ...
White papers
14 Aug: Missing Bills: Are You Getting Paid What You’ve Earned?
Ingenious Med makes it a priority to help healthcare organizations quickly identify missing charges in a number of ways so they ca ...
Blog
13 Aug: 3 Tips to Reduce Missing Bills
With so much variation and so many people with the opportunity to touch each charge, it’s easy to see how some are missed. Makin ...
White papers
18 Jul: Optimizing Net Revenue
As a healthcare provider you are confronted with the challenge of competing profitably in an industry where reimbursements are bec ...
Blog
11 Jul: Calculating the Economic Benefits of Effective Charge Captur...
According to the 2016 Revenue Cycle Management Report, a survey of 2,000 independent physician practices and 200 hospital-based ph ...
White papers
10 Jul: Optimizing the Revenue Cycle Starts Here
There is nothing more elemental to healthcare than a physician’s treatment of a patient. As much as the industry continues to ev ...
Blog
21 Jun: How the Effects of Under-Coding Have Gone from Bad to Worse
Now more than ever, data counts. “The revenue of many healthcare provider organizations is inexorably tied to charge capture. Th ...
Blog
07 Jun: Why Effective Charge Capture Has Never Mattered More
Unprecedented Margin Pressure
For reasons ranging from shrinking Medicare rates to the continued shift of inpatient care to out ...
Case study
22 May: Doc Image Capture Case Study
CMS and commercial payers are all getting better at analyzing large volumes of claims data – that’s why it’s critical that h ...
Blog
08 Mar: Four Tips to Be a Better Steward of Opioid Prescriptions
The opioid epidemic is being called the worst public health crisis in America. And the numbers keep rising. I can remember a time ...

White papers
27 Apr: Technological Solutions To Coordination Of Care
The following white paper will be available for download upon filling out the form below:
Technological Solutions to Coordinati ...

Blog
30 Mar: The Transition to MACRA: Six Best Practices for Inpatient Qu...
As published by HealthIT and mHealth
By Stephen Besch
Senior Systems Analyst, Director of Clinical Quality Reporting
The Q ...
Blog
15 Mar: Change and Inadequate Tools Pose New Challenges for Physicia...
As published by HISTalk Practice
By Joe Marabito, Ingenious Med Chief Executive Officer
Physicians are the most important elem ...

Blog
27 Feb: Ingenious Med Named a TAG Top 40 Innovative Technology Compa...
Ingenious Med was named one of Georgia’s Top 40 Innovative Technology Companies by The Technology Association of Georgia (TAG). ...
Case study
08 Feb: Emory Healthcare Case Study
Emory Healthcare, the largest healthcare system in Georgia, is a multidisciplinary medical organization compiled of six hospitals ...
Case study
08 Feb: Schumacher Group Case Study
The Lafayette, La.-based Schumacher Group, a large multi-state provider of emergency department and hospitalist services, has been ...

Blog
17 Oct: The Need for Evidence-Based Health Care
The amount of data in any given hospital or physician practice is staggering. Patient records, billing information, compliance fi ...
NEWEST WEBINAR
Re-energizing value-based care: The strategies physicians & health systems need to succeed
