By Felice Felser, MBA, MSN, APRN, Senior Product Manager
The opioid epidemic is being called the worst public health crisis in America. And the numbers keep rising. I can remember a time in nursing school where we were taught to treat pain as the “fifth vital sign.” We were told not to question the patient’s perception of pain but to treat accordingly as many felt that patients were often under-medicated.
I brought that mentality and school of thought into my profession as an Emergency Room nurse and later as an Emergency Room Nurse Practitioner. What I saw over the 10-year period of time was quite astonishing. The cry for narcotic pain medication like Vicodin and Percocet was constant. The stories conjectured in order to obtain opioids were amazing. The lengths the addicted would go to obtain their drug was bewildering. I began to know some patients by name as I saw the same people daily, weekly. They came to the ER seeking refills of what other providers would no longer prescribe. Some days I felt the Emergency Room was just a large pharmacy, misused and abused. If we refused to write a narcotic prescription, we ran the risk of receiving poor Press Gainey scores from dissatisfied patients or reduced reimbursements by CMS whose survey asked whether “your doctors did everything they could to help with your pain.”
As the years passed I transitioned to urgent care and thought things would improve. Although the epidemic had worsened over the years, providers were asked to check the state-wide drug registry if we suspected opioid abuse and look for multiple prescriptions from various physicians or what we called “narcotic shopping.” Many physicians also received bulletins from the FDA as well as from insurance providers who were co-paying for the prescriptive narcotics. This proved to be helpful and one by one, we began turning down narcotic prescription requests while offering alternative pain management regimens. There was a marked decrease of opioid abuse at the facility where I worked due to the diligence of the providers. Unfortunately, for every provider who sought a greater level of knowledge through the drug registry, there were equal numbers who took the easy way out.
Now, we are faced with an even bigger problem – one that has manifested over the years to reach epidemic proportion. Opioid abuse not only consists of the massive proliferation of prescription painkillers, but also drug overdose and death from heroin and fentanyl. It predominates in rural areas of America but has also hit the wealthy and famous. It is the reason we have lost numerous icons as well as physicians that I have worked with over the past years.
Opioid abuse in the United States is responsible for more $78 billion a year in healthcare costs, lost productivity, and addiction treatment. It claims more than 115 lives per day and the number is still increasing. It is incumbent upon physicians and practice management groups to continue to take active roles in opioid abuse utilizing innovative technology on the market to make it possible.
Tips for Reducing Opioid Prescriptions
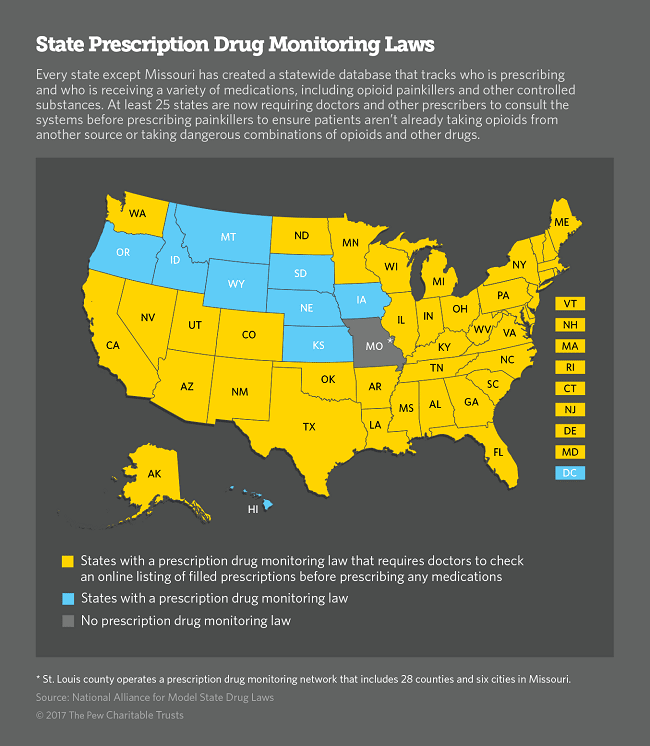
- Check the state Physician Drug Monitoring Program database to learn state laws and rules for opioids in order to identify, deter, and prevent drug abuse.
- Understand if you are required to check the PDMP map before prescribing opioids – as of October 16, 2011, 37 states have operational PDMPs that have the capacity to receive and distribute controlled substance prescription information to authorized users.
- If you prescribe opioids, limit the number of pills prescribed at any given time and require patient check-ups before prescribing more. From an ER perspective, we limit prescriptions to a quantity of 12 or 15 with no refills.
- Try alternative non-narcotic pain regimens and refer people appropriately to pain clinics that provide personalized treatment plans for chronic and acute pain when needed.
Today, there are still no incentives for physicians to help control opioids, but in some states, legal penalties are being assessed. Physicians and management groups have taken it upon themselves to act as better stewards of opioid prescriptions. Some groups are developing provider-level quality measures around opioids and are interested in considering new measures and best practices for quality improvement. To assist the medical community, there is also innovative technology relevant for physician and hospital practices which automatically flags those patients who have been diagnosed with opioid abuse. In this manner, providers will have an immediate, visible indicator that will help guide their clinical decision pathways and alternative pain management regimens. This will help increase a patient’s quality of care, reduce waste within the healthcare system, and decrease the potential of associated penalties.
Want to see more? You can find our other blogs here.
Don’t miss out on our next blog! Subscribe here.