One of the most effective ways to improve a healthcare organization is to learn from other successful organizations. Healthcare leaders should continually evaluate what makes their competitors thrive, and then incorporate similar strategies.
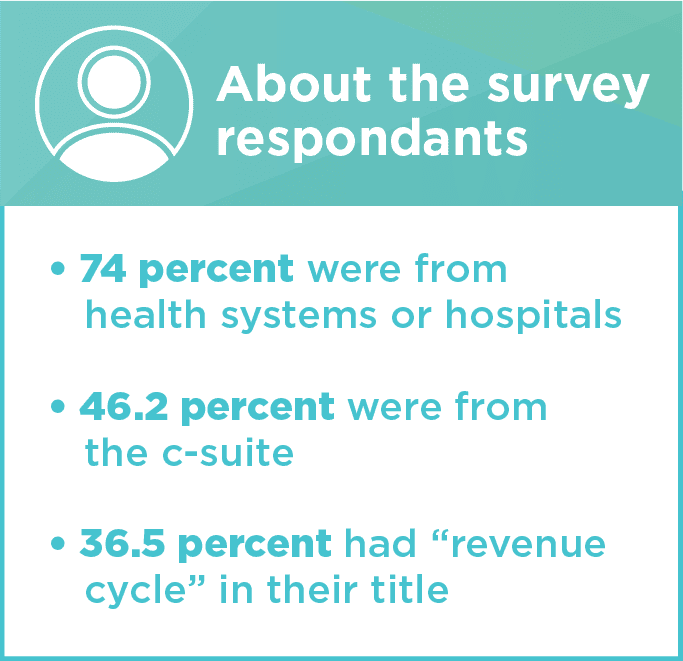
To help organizations get started, specifically when it comes to improving revenue cycle management (RCM), Ingenious Med recently surveyed 104 healthcare executives to establish the current state of charge capture. Then, it identified the top 20 percent of respondents as top performing organizations, based on their responses to questions related to six metrics:
“These metrics helped us identify the organizations with the most efficient revenue cycles, fewest denials, and most accurate coding,” says Bryan Goble, Director of Product Management, Ingenious Med. “All of these factors translate to a healthier bottom line.”
How much healthier? The impact of a more effective revenue cycle management system could be significant. The average 350-bed hospital misses $22 million in revenue capture opportunities, according to a report from the Advisory Board Company, a healthcare consultancy.
“Organizations must focus on top-line growth by capturing all charge opportunities and address understated coding which can be a game changer for many health systems and hospitals.,” says Steven Liu, M.D., SFHM, Founder and Chief Medical Officer, Ingenious Med. “By recording the care actually delivered in a timely manner, we have the power to impact revenue by ensuring the organization is billing accurately for services truly rendered. The status quo is no longer an option.”
Important Takeaways
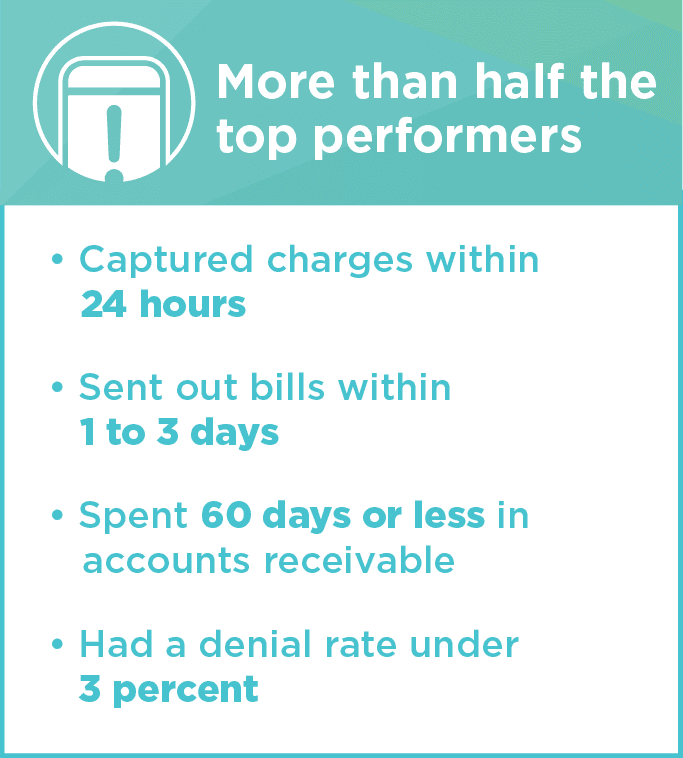
Ingenious Med used its survey responses to identify common characteristics that high performer respondents shared when it came to revenue cycle management.
It found that 72 percent of respondents from organizations classified as non-top performers said missed charges are a top issue with their current charge capture process. Only 26 percent of top performers said this was a top issue.
This indicates, of course, that top performing organizations have found a way to reduce their number of missed charges. This helps their bottom lines, and it also means they have more time to focus on other important tasks, such as decreasing charge lag, conducting data analyses to monitor trends and performance, and providing real-time data to physicians so they can improve their charge practices.
“When we really embraced the missing bills functionality within Ingenious Med to its fullest, I had an employee come tell me that a process that was taking her a day and a half, was now taking her two hours,” said Monica Wright, Director of Compliance and Clinical Documentation Improvement at Adfinitas Health. “Anytime that you can make that kind of change in the efficiency of the organization, it helps you focus on other, more important issues.”
While we went into some detail about the Three Tips to Reduce Missing Bills in an earlier blog post, it is important to dive deeper into the benefit of having a dedicated charge capture solution that finds, marks, and resolves missing charges quickly and within the normal workflow.
Which Systems Work Best
Most organizations, according to the survey findings, rely primarily on EMRs for charge capture, though many are still using paper processes as part of their system.
While having an all-in-one EMR/charge capture solution would seem to make the most sense in locating and dealing with missing charges, the truth is that no software can do it all, says Felice Felser, Director of Portfolio Management & Analytics, Ingenious Med.
“When it comes to EMRs, especially for integrated systems with multiple EMRs, interoperability problems increase the likelihood of missed charges,” she says. “Relying on a paper system for charge capture results in other problems. When physicians track charges on paper and then enter information into the EMR later, information can be incomplete or missed altogether.”
The survey findings underscore this problem. Of the respondents who said they use an EMR, a paper system, or a combination of EMR and paper for revenue cycle management, all cited missed charges as their number one challenge.
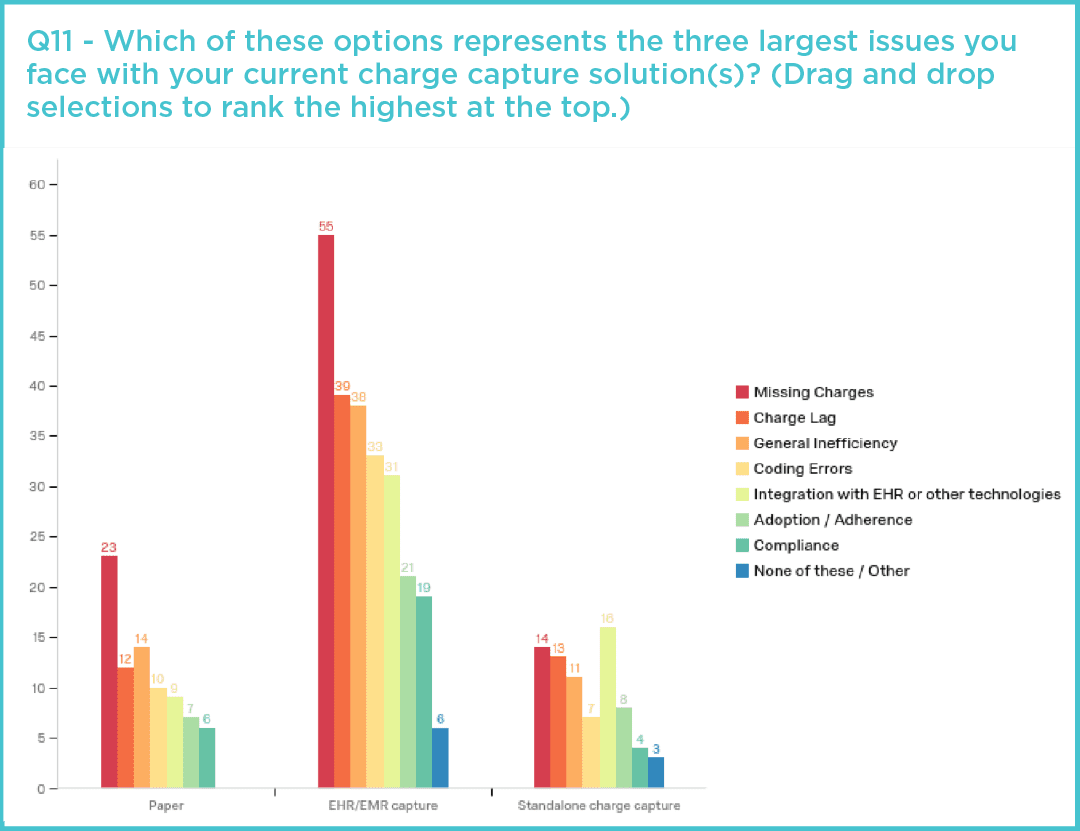
The only group who did not cite it as a number one challenge were those who said they primarily use an electronic standalone system.
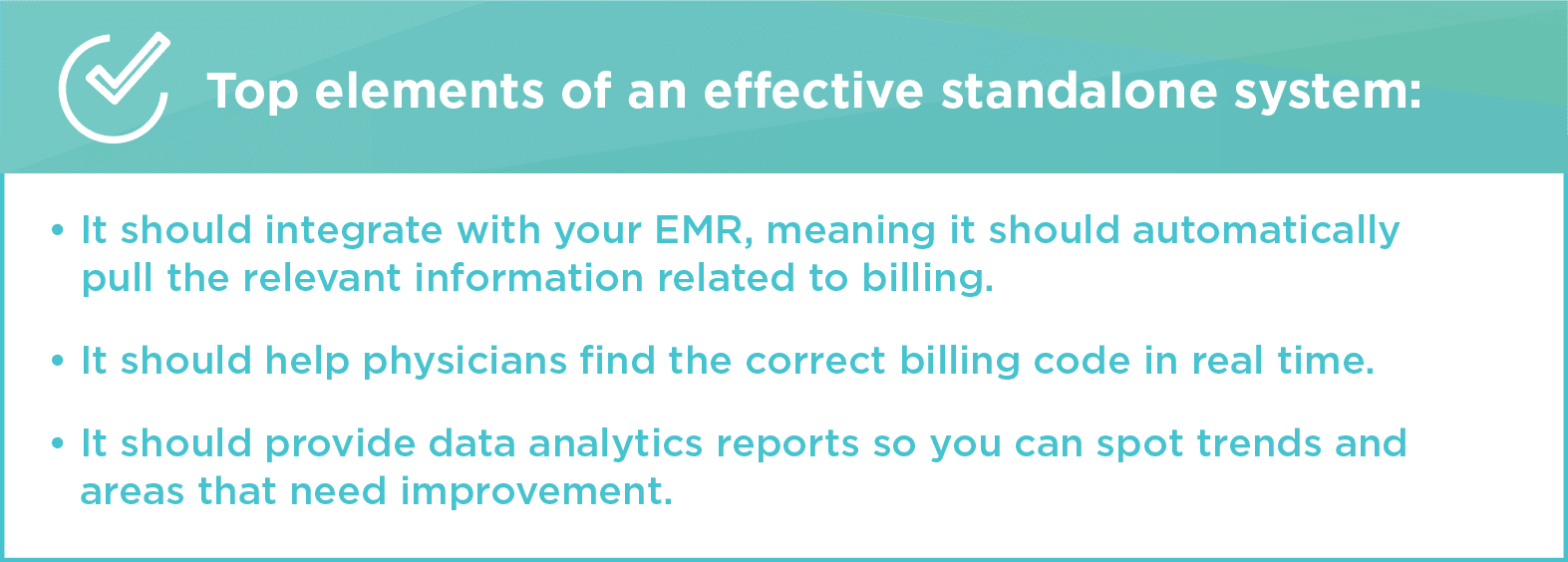
Standalone systems are built more specifically for capturing and recording charges among multiple locations and groups. That means charges aren’t missed due to EMR integration problems or lost paper notes. The best standalone systems have integration solutions for multiple EMRs, creating a single source for bill tracking. These systems help organizations proactively identify missing bills because all charge information is kept in one place.
“In the past, it could be two months before we realized we had missed a charge,” says Anne McMorrow, Director of Reimbursement at iNDIGO Health Partners, a physician-led company that works with community hospitals and post-acute care facilities to provide hospitalists, locum tenens, telehealth, and other services. “Ingenious Med makes that process more timely. With timeliness comes accuracy. We know the charges that we’re capturing with Ingenious Med are more accurate.”
For more information about how missing bills can affect your organization, please read our whitepaper, Missing Bills: Are You Getting Paid What You’ve Earned? In the next blog, we will be wrapping up our Top Performers series, discussing the multiple ways that hospital leaders can more effectively manage RCM.