Every part of the revenue cycle is vital to an organization’s financial health, yet not every aspect is treated equally. The coding process is often written off as a necessary but messy process, accepting that care providers don’t have sufficient time to document everything at the time of care. Fortunately, there is a better path forward, but it will involve dealing with three areas of the coding process: workflow efficiency, compliance, and physician work relative value unit (wRVU) improvement.
Workflow efficiency
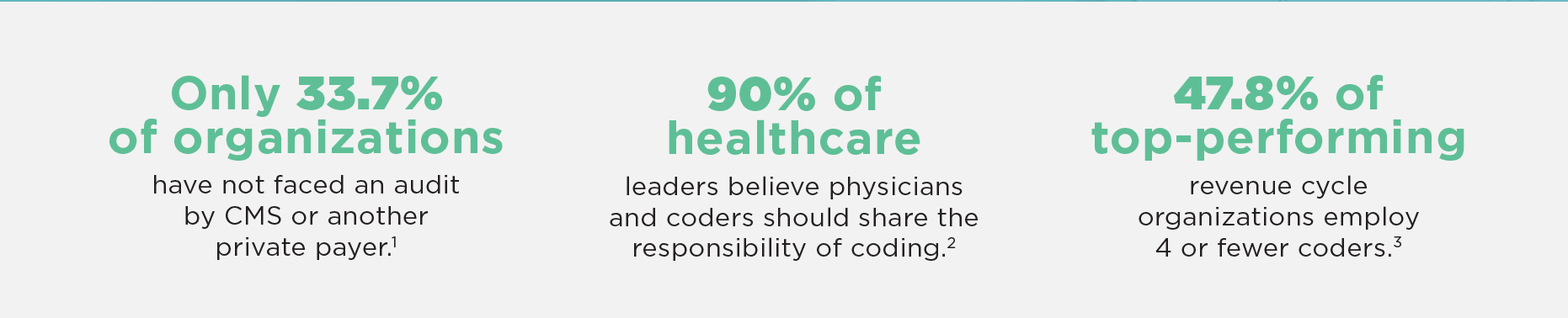
There is a symbiotic relationship between the care providers and coding department. Without cooperation from both parties, bills cannot be accurately sent out. Even with this knowledge, there’s often disagreement on where the majority of coding responsibility lies. Many physicians don’t regard coding as a responsibility that falls under their purview, instead relying on coders to do the heavy lifting. And yet, according to a recent Ingenious Med study, only 23 percent of healthcare leaders believe that the coder is more responsible than the provider for accurately capturing medical services for billing.4
This dichotomy between providers and leadership leads to unnecessary coder follow-up to verify the accuracy of data and supporting documentation before submitting a claim. Over half of organizations believe their coders spend between 10 – 25 percent of their time tracking down information from physicians.5 That’s potentially hours wasted every single day. As coders spend more time reaching out and waiting for responses to billing questions, fewer bills can be completed.
Compliance
While workflow efficiency is a slow leak, the greater flood risk comes from compliance. The coding process is fraught with the risk of compliance penalties due to improper coding. Federal regulators are increasingly focused on the accuracy of medical billing, while at the same time private payers are becoming more adept at analyzing large volumes of claims.
The recent introduction of the Targeted Probe and Educate (TPE) program by the Centers for Medicare & Medicaid Services (CMS) is evidence of the federal government’s redoubled commitment to compliance. Red flags ranging from billing data that is indicative of potentially “questionable billing practices” to services that have high national error rates can all trigger a Medicare audit. These audits can result in stiff fines if organizations do not make the necessary changes and improvements.
How does MasterCoder work?
Ingenious Med’s MasterCoder functionality assists care providers with their selection of the correct E&M code at the time of bill creation. If enabled, MasterCoder functions much like a “wizard”; its purpose is to walk care providers through the necessary criteria to meet E&M service levels for successful billing.
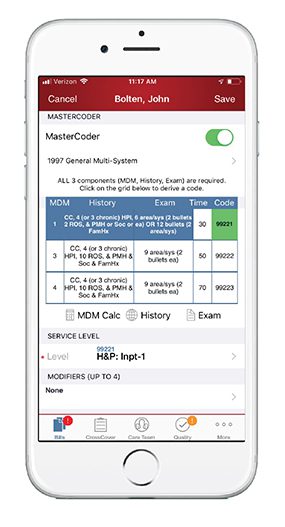 MasterCoder consists of both the 1995 and 1997 documentation guidelines which are acceptable for Medicare carriers.
MasterCoder consists of both the 1995 and 1997 documentation guidelines which are acceptable for Medicare carriers.
The documentation grid utilizes a Medical Decision Making (MDM) calculator in order to derive a suggested service level code. The MDM calculator takes under consideration the nature and number of diagnoses, the patient’s risk of mortality and morbidity, and level of complexity as entered by the physician in order to assign the proper MDM number. The MDM is then utilized by the physician in conjunction with chief complaint, history of present illness, review of systems, and number of exam bullets in order to assign the proper E&M code.
Physician wRVU improvement
Improper coding has a negative affect on the overarching healthcare institution — but it also can have an adverse impact on the providers themselves. While the increase in value-based payment has begun to factor into physician compensation, wRVUs are still by far the most prevalent part of any compensation metric.6
Providers have been under-coding for the services that they are performing for a number of reasons, including time constraints, lack of training, or a desire to not overcharge patients. But as providers learn to code appropriately, they will help the overarching healthcare institution — and optimize their own take-home pay.
With these three issues in mind, Ingenious Med built MasterCoder to assist care providers with their selection of the correct E&M code at the time of bill creation. While MasterCoder does not replace the need for doctors and coders to correctly chart and document charges, it is an effective tool to increase coding accuracy and optimize coding efficiency.
MasterCoder has been proven to improve the three-part issue from improper coding:
- Greatly improves the consistency of proper coding at the point of care, saving coders valuable time.
- Minimizes errors that result in over- or under-coding on an insurance claim, preventing red flags for external audits and protecting against costly compliance penalties.
- Increases the overall dollars per wRVU across an organization. According to Ingenious Med records, bills using MasterCoder resulted in 12 percent higher RVUs than those not using it.
Furthermore, unlike EHR black box systems, which calculate codes behind the scenes based on your electronic notes, MasterCoder is transparent about what levels of documentation and services are required. This can help prompt providers who might have omitted a service to add it in, allowing them to bill for a higher level of service. While EHR systems are often a single mouse click to code, without the transparency of the process, it can still leave providers with inaccurate coding.
Overall MasterCoder Use
Looking at the entire business in 2018, Ingenious Med has analyzed all of its clients’ charge capture coding data to discern patterns in coding efficiency and accuracy. While this analysis goes into great detail about a wide variety of measures, we are concerned primarily with two factors concerning MasterCoder usage:
- MasterCoder is on and the suggestions are used (ON)
- MasterCoder is off or the suggestions are not used (OFF)
While all organizations are different in terms of how often they are mandated to use MasterCoder, how many codes they may use in the practice, and how the final bills are coded and submitted, there were a number of trends that can be seen.
Ingenious Med found that the coding accuracy was highest when MasterCoder was on and the suggestions were used.
While using the MasterCoder suggestion, only 1.6 percent of bills required up-coding, compared with 4.1 percent when MasterCoder was off.
Using MasterCoder had similar results when looking at the down-coding and series changes as well.7 Users recorded an average of half as many changes required for those coding categories.
While looking at the macro scale provides some top-level highlights, Ingenious Med took a look at two examples from their study from January 2017 to March 2018 to better highlight individual performance results.
Case Study #1
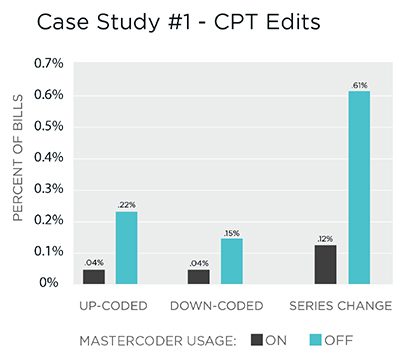
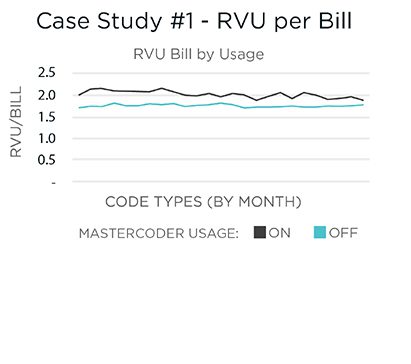
A five-hospital system with over 200 users. The providers span several specialties but are primarily hospitalists. The organization began using Ingenious Med in December 2015. Since implementation, MasterCoder was set at 20 percent for all providers, meaning that one in five captured charges would activate MasterCoder to assist in the accurate code selection. In addition, some providers opted to have the program turned on for all bills, resulting in an overall usage of 51 percent.
As part of the utilization study, Ingenious Med analyzed over 242,000 bills. The result clearly demonstrated that ON charges were much more accurate and resulted in higher billing:
- Only 53 (0.04%) bills using MasterCoder were up-coded on the back end. OFF bills were adjusted nearly 6 times as often for up-coding.
- Similar rates of change can be seen for coding series changes, jumping from 140 (0.12%) for ON codes to 741 (0.62%) for OFF codes.
Furthermore, during that time ON charges resulted in 12 percent higher RVUs per bill than all of the OFF charges. At a $4.30 increase per RVU, this could mean that OFF bills could be leaving around $1.68 million on the table. While this organization did not have plans to require an increased, mandatory limit on MasterCoder usage, the organization has realized significant financial and optimization gains from their current usage.
Case Study #2
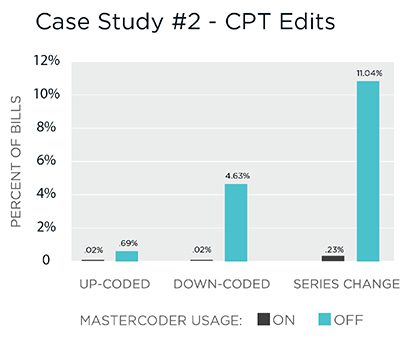
A 500-physician, non-profit health system with a comprehensive set of services.
During the survey timeline, Ingenious Med surveyed 139,242 bills, with an overall usage of MasterCoder at 27 percent.
This organization saw very dramatic differences between the ON and OFF bills, with very low changes for up-coding, down-coding, and series changes when MasterCoder was used:
- 30x less up-coding on bills, comparing ON to OFF bills (0.02% – 0.69% of bills)
- OFF bills saw a 4.6 percent down-coding rate, while ON bills were at a miniscule 0.02 percent
- Series change was the most dramatic category, with 11 percent of OFF bills requiring a series change, while ON bills were at less than one quarter of one percent.
As the organization continues to expand its charge volume, this optimization will help to mitigate the need for additional expansion in coding capacity.
Conclusion
MasterCoder is not meant to be a cure-all for inefficient coding. But with over two-thirds of healthcare organizations believing that more than 1 percent of their charges are under- and over-coded, this leaves a lot of money on the table for services that are already being provided. On either a large or small scale, through judicious use of the tool, an organization can yield incredible results in mitigating losses from chronic under-coding and compliance risk from over-coding.
Understanding the hectic nature of physician schedules, Ingenious Med recommends periodic use of MasterCoder rather than for every encounter. Organizations use a variety of preference settings to fit the needs of their unique situations. Some require all new physicians to use it for their first 90 days and for all residents. Some mandate use after a physician fails an audit. Others find it useful to have all providers use MasterCoder for a certain percentage of bills.
During implementation, Ingenious Med will work with a group or practice to identify, customize, and configure MasterCoder settings for care providers as appropriate.
For best results, Ingenious Med suggests that MasterCoder usage should be considered by the following groups/practices:
- Those who wish to assist care providers with charge entry.
- Those who wish to limit over-coding and under-coding.
- Those with care providers who are unfamiliar with E&M service level requirements.
- Those who have not captured E&M service level charges previously.
- Those with auditing or tracking measures in place for onboarding new care providers.
- Those with auditing procedures in place for care providers to check for over-coding and to improve revenue generation by avoiding under-coding.
- Those with students and/or residents (new care providers) with no billing experience.
For more information about MasterCoder and other features of Ingenious Med, request a demo today at www.ingeniousmed.com/demo.