With everything healthcare executives need to keep an eye on, revenue cycle management (RCM) performance — and specifically charge capture — sometimes doesn’t get as much attention as it deserves.
But a more effective RCM system could have a huge impact on a hospital’s bottom line. In fact, a recent report from the Advisory Board Company found that the average 350-bed hospital misses $22 million in revenue capture opportunities.
But while under-coding and missed charges present significant financial risk for health systems, they aren’t the only problems healthcare executives need to be aware of. Over-coding can lead to overpayments, which can result in significant penalties.

In one recent case, the Office of Inspector General (OIG) stated that Madison, Wisconsin-based University of Wisconsin Hospital and Clinics submitted erroneous bills to Medicare, and needed to refund the Medicare contractor $2.4 million. In another case, the OIG stated that New York-based Mount Sinai Hospital owed the government nearly $42 million for improperly billed Medicare claims.
The good news is there are some small steps healthcare executives can take to ensure their hospital is capturing the right charges — and not the wrong ones. Here are five tips:
1. Discuss charge capture more often with RCM leaders and clinical leaders.
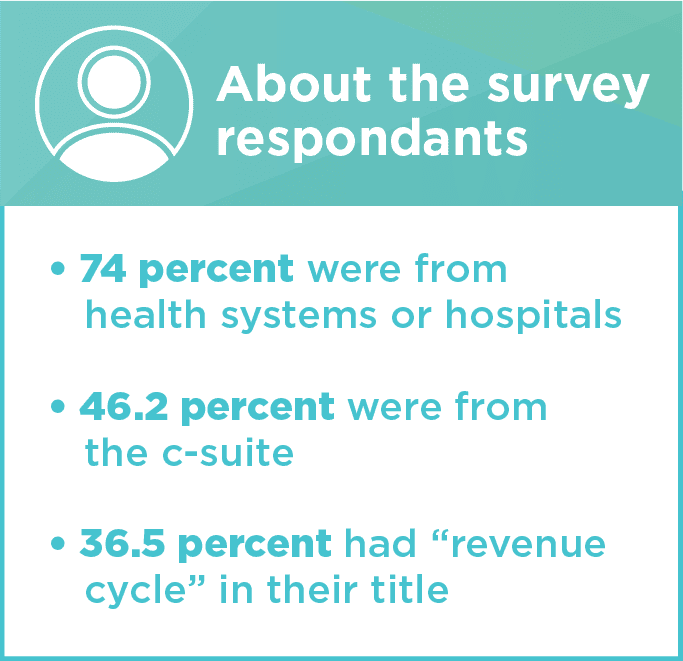
Given the impact charge capture can have on a hospital’s bottom line, it would be natural to assume that senior leaders discuss it regularly during meetings. But a recent survey by Ingenious Med of more than 100 healthcare leaders found that while over three-quarters believe charge capture is essential to their organization’s success, nearly half meet only once a month or less to discuss charge capture.
View full survey findings, here.
Discussing charge capture more often with senior leaders, RCM leaders, and physician leaders can have a big impact on charge capture. One of the biggest reasons? It sends the message to clinical and coding staff that charge capture is a priority at all levels of the organization Once that’s clear, everyone can work with a common goal in mind.
Keep in mind that discussing charge capture more often doesn’t mean hospitals need to have a formal charge capture meeting every week. But they should at least include RCM as an agenda item during key leadership meetings, and the appropriate individuals should be invited to provide an update on how the RCM process is going.
2. Make it easy for physicians and staff to raise concerns.
If senior leaders don’t know what the problems/barriers are to effective charge capture, improvements will never be made.
Physicians and staff who are capturing charges on a daily basis must have the ability to raise concerns and ask for more resources when necessary. Some approaches to consider include:
- Forming a focus group of clinicians and billing staff (with representation from each department), that meets quarterly to discuss charge capture challenges and then brings those challenges to senior leadership.
- Creating a virtual feedback system or virtual chat system so that when clinicians encounter RCM challenges, they can ask for help from experts. If the experts can’t help, they should bring the problems to senior leadership. At the very least, communication between clinical and RCM staff should be electronic and real-time.
3. Make sure RCM leaders share performance feedback with clinicians.
If clinicians don’t know what they are doing wrong, it’s impossible for them to improve. Make data transparency a priority, and ensure physicians have insight into their own performance when it comes to charge capture.
Send them monthly or quarterly reports so they can see how they are doing. To capitalize on their inherent sense of camaraderie and competition, show them how they are performing relative to their peers.
For tips, read 4 Questions to Answer with Physician Performance Metrics.

4. Monitor metrics.
Don’t wait for an OIG audit to find out there’s a problem with charge capture. Proactively monitor how your hospital is performing against key RCM metrics.
Not sure how to get started? After completing its survey, Ingenious Med used the results to identify the top performing organizations when it came to RCM. It found that:
- More than 50 percent of top performers capture charges within 24 hours.
- 70 percent of top performers send out bills within one to three days.
- Most top performers have an average duration in accounts receivable of less than 30 days.
- Most top performers have less than 1 percent of their charges under-coded and over-coded.
- Most top performers have a denial rate less than 3 percent.
These metrics should serve as a good starting point to determine how a hospital is doing compared to top performers, and where it needs to make improvements.
5. Rethink the current charge capture solution.
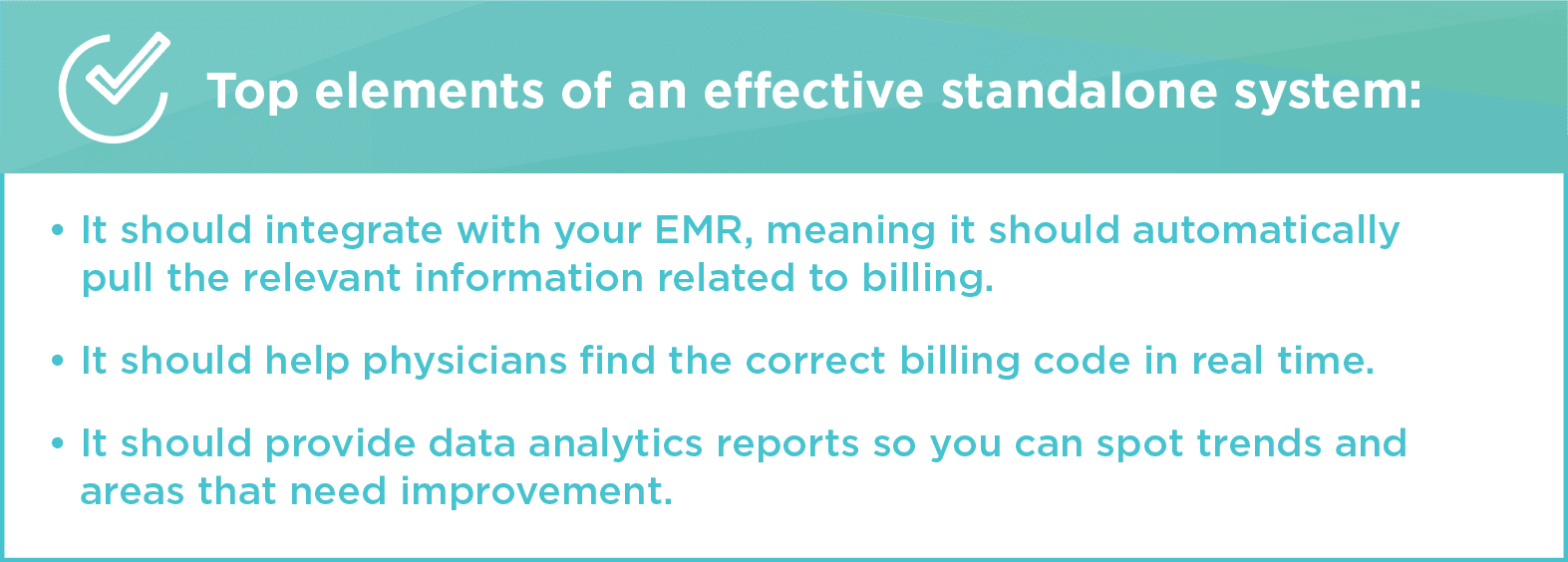
Over half of respondents to Ingenious Med’s survey indicated a high level of dissatisfaction with their current charge capture system. The survey also found that most respondents rely on an EHR or an EHR/paper workflow to capture charges.
For organizations that use these methods, a standalone, electronic charge capture option may be a better fit. The survey reveals that the only group of respondents who did not cite missed charges as a top challenge with their RCM system were the respondents who said they use a standalone system. This is because a standalone system makes it easier to capture charges across multiple locations, groups, and EHRs.
How much revenue might you gain with better charge capture? Request an Ingenious Med demo today.
Want to see more? You can find our other blogs here.
Don’t miss out on our next blog! Subscribe here.