Practical steps to enhance reimbursement, revenue capture and physician productivity
By Lynn Mettler, Client Delivery Officer
Even before COVID-19 hit, hospitals were struggling to make ends meet with nearly a third operating at a loss. The AHA reported that, as of June of this year, hospitals and health systems were seeing average reductions of nearly 20% in inpatient volumes; it projected average losses of over $20 billion per month through the end of 2020.
Our own data revealed a significant decline in bill volumes starting in March 2020. While volumes began to recover in the summer, they have modestly declined again as the number of new cases climbs. Instead of being able to put COVID behind us, we continue to need strategies that address its many challenges.
That makes the insights shared at our recent webinar with two healthcare leaders – Derick D. Perkins, Founder and Managing Partner of Metis Advisors LLC and Dennis Deruelle, MD, Executive Director of Hospital Medicine at American Physician Partners (APP) – of continuing relevance as we move into the winter. This blog highlights five tactics they shared to manage reimbursement changes, revenue capture and physician productivity during the pandemic that you can incorporate into your own planning.
 Where Changes Affect Financial Viability
Where Changes Affect Financial Viability
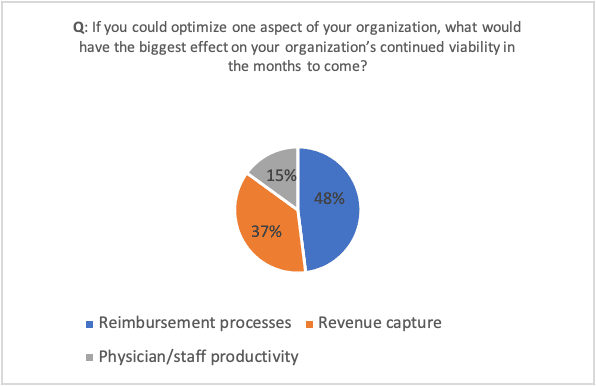
A poll we conducted during the webinar found that nearly half of the respondents (48%) selected optimizing reimbursement processes as most important to their financial viability, while 37% selected optimizing revenue capture and 15% chose optimizing physician and/or staff productivity as most important.
These tactics rely on being able to accurately capture charges and COVID patient data in real time and being able to tie that data to physician staffing and compensation, claims submission and value-based care programs.
1. Proactively adapt to a changing payer mix
While hard data is not yet available, the number of uninsured individuals is estimated to have increased by 3 million to 8 million as a result of the pandemic. To address this increase, our panelists recommended having a comprehensive self-pay strategy that can identify which patients will need to pay out-of-pocket for some (or all) of their care, as well as tools that estimate patient costs upfront. Ideally, organizations should also make their charges more transparent and enable patients to pay online and take advantage of financing options like medical credit cards that allow them to spread payments out over time.
COVID also increased the volume of Medicaid and Medicare patients at many facilities while pediatric and commercially insured patient volumes plummeted. Since government insurers typically reimburse at about half the rate of commercial insurers, the pandemic makes it more critical than ever to fully capture charges while containing costs. Dr. Deruelle and Mr. Perkins noted that having a shared mobile charge capture solution at the point of care helps ensure timely and accurate documentation of all services rendered, including making it easy for physicians to capture any comorbidities with ready access to diagnostic codes in their specialty.
2. Identify and isolate COVID-19 patient data for accurate value-based care metrics
Participants in the BPCI Advanced program should be able to exclude COVID patients from their bundled payment metrics in order to make an informed decision about whether to stay in the program’s two-sided risk model for two quarters this year or take advantage of program amendments. APP used the Ingenious Med® application’s identifiers and trackers to know exactly which patients had COVID, and factored that into their calculations about the ideal BPCI Advanced strategy.
3. Have a shared billing platform across facilities
Having a common billing platform across multiple locations allows physicians assigned to work in unfamiliar hospitals and clinical areas during COVID surges to bill efficiently and accurately regardless of location. APP also used the Ingenious Med solution to help physicians capture charges for unfamiliar types of services – from virtual visits to critical care – and identify missing bills on a daily basis so they could remind the appropriate physician to enter missing charges.
4. Provide physician education and incentives
Our panelists also found that providing physicians with robust coding education enabled their coders to move to more of an auditing role while also increasing revenues. The MasterCoder function in the Ingenious Med application proved useful to help clinicians enter the correct A&M codes.
Providing physicians with incentives or penalties for timely and accurate billing can help healthcare organizations achieve the desired results. Mr. Perkins noted the success of implementing a policy that penalized physicians who failed to enter charges within 10 days of service delivery.
5. Leverage analytics to adapt physician workloads and compensation due to COVID patient impacts
The pandemic makes it essential that organizations track patient census information in real time on a daily basis. APP used data in the Ingenious Med application’s dashboard to track the number and location of COVID patients. When an area had a high volume of COVID patients, it lightened the typical hospitalist workload to provide adequate time to don and doff PPE, communicate with family members and provide additional care. The data also helped APP redeploy staff from lower to higher need areas, with additional physician resources available via virtual visits and a team of on-call physicians in the event of sudden surges.
Mr. Perkins recommended that healthcare organizations adjust physician bonus targets to accommodate the fact that COVID patients impact productivity.
The experience of these two healthcare organizations demonstrates the power of point-of-care solutions for capturing charges and tracking volumes. Sadly, the accelerated need for the tactics shared here is not yet behind us, with COVID resurging in much of the country. Even once the threat of COVID has receded, these solutions can help organizations keep costs down while optimizing revenues.
To listen to more of the discussion, you can view our recording of the webinar. You can also read our white paper, “Rising to the Challenge: How Leading Healthcare Organizations are Thriving in an Evolving Revenue Environment,” which explores these strategies in greater depth.