Unprecedented Margin Pressure
For reasons ranging from shrinking Medicare rates to the continued shift of inpatient care to outpatient settings, health systems and hospitals are under unprecedented pressure to improve their operating margins.
According to a FY 2016 analysis by Moody’s Investors Services of 323 not-for-profit and public-sector hospitals and health systems, the annual expense growth rate of 7.2 percent outpaced the annual revenue growth rate of 6 percent.
More recently, the ratings agency downgraded the sector in a December 2017 announcement: “Operating cash flow declined at a more rapid pace than expected in 2017, and we expect continued contraction of 2 to 4 percent through 2018.” Healthcare enterprises are spending more than they’re growing.
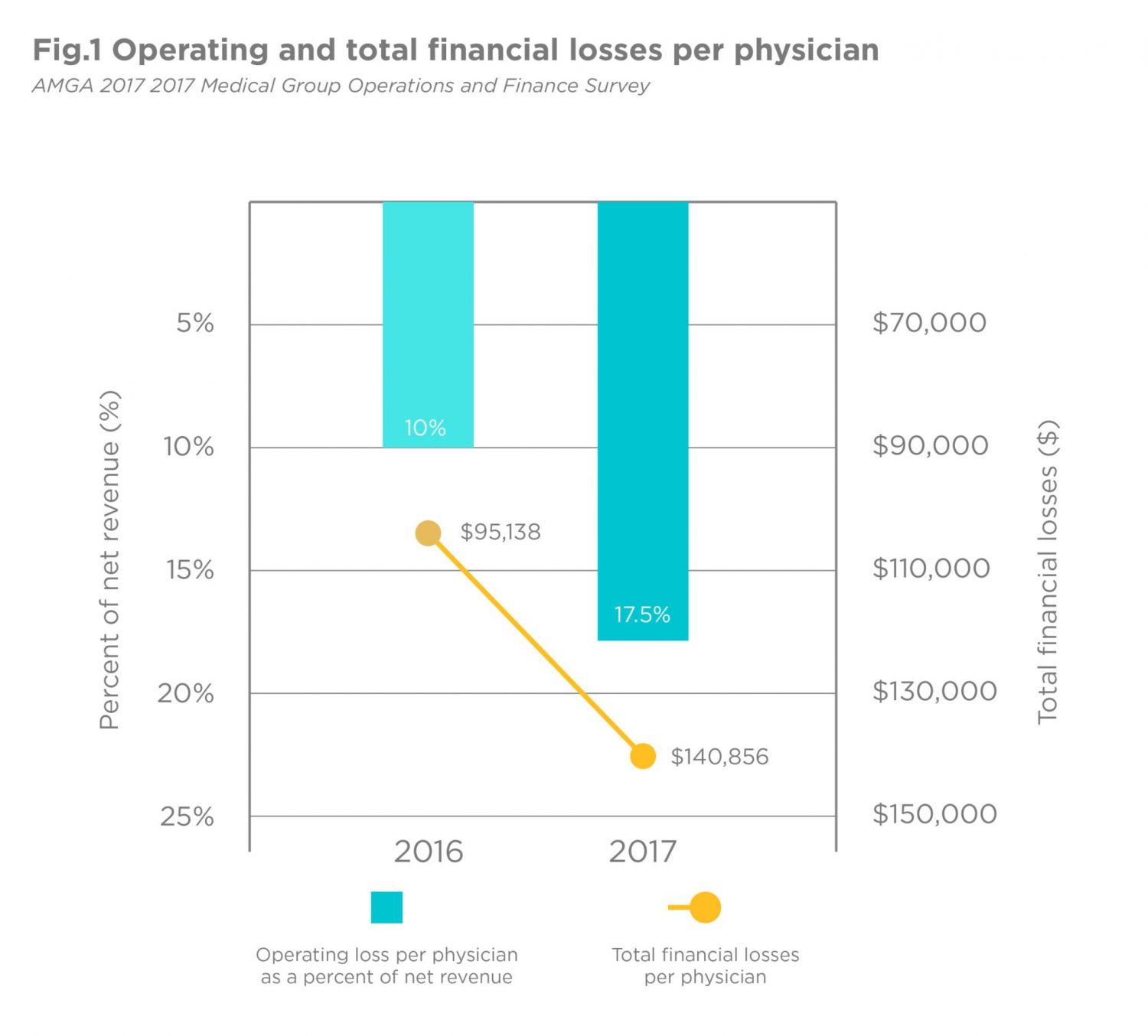
Many health systems and hospitals have responded to this financial pressure, attempting to add additional revenue streams by acquiring physician groups — a business they have historically struggled to manage cost-effectively (as the Fig. 1 infographic illustrates).
The trend has become so pronounced that, according to an American Medical Association study, only 47.1 percent of physicians in 2016 had ownership stakes in a medical practice. That’s down from 53.2 percent in 2012. This milestone marks the first time that the majority of physicians are not practice owners.
Enhancing Operating Margin Through Charge Capture
Increasingly, health systems and hospitals are reassessing their revenue cycle management processes to eliminate operational inefficiencies, while identifying services for which they can be better compensated. As a result of this focus, charge capture is emerging as a prime tool for many healthcare organizations in enhancing the operating margin.
“Cutting your way to success is no longer an option for healthcare organizations. Many have already implemented major cost-cutting programs over recent years,” said Steven Liu, MD, SFHM, founder and chief medical officer of Ingenious Med. “Organizations must also focus on top-line growth by capturing all charge opportunities and address understated coding which can be a game changer for many health systems and hospitals.”
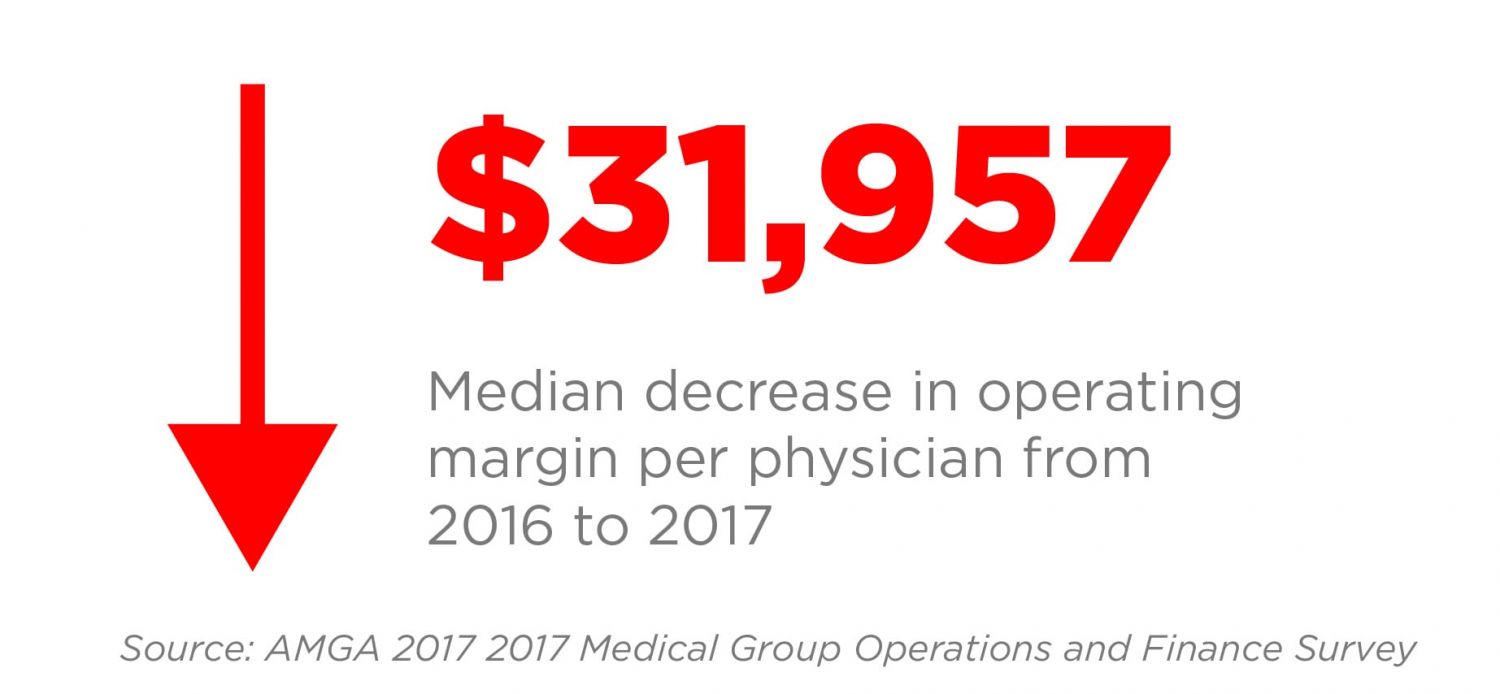
Lost revenue stemming from services rendered by individual physicians not being accurately recorded is a challenge confronting many healthcare provider organizations. According to a 2017 AMGA survey of 49 organizations representing more than 13,000 physicians, the losses stemming from services provided by individual physicians is significant:
- The operating loss per physician increased from a loss of 10 percent of net revenue in 2016 to a loss of 17.5 percent of net revenue in 2017.
- Total financial losses per physician during this two-year period went from $95,138 to $140,856 per physician at the median.
- During this period, despite gross professional revenue increasing from $1,217,350 to $1,328,625 at median, net professional revenue actually decreased at median from $682,735 to $681,322 — all but eliminating the revenue gains.
Get Paid for What You Do: Starting with an Increase in Charge Quantity
Charge capture — a process that once entailed clinicians manually recording their interactions with a patient on a chart — has become incrementally more automated in recent years. Then and now, however, charge capture’s effectiveness has relied largely on physicians adapting to processes that many of them find tedious.
“As a physician, I would often question why traditional charge capture needed to be time-consuming and if there wasn’t an easier way to obtain such data in a clinician-friendly way,” said Liu. “Ultimately, I recognized that there was indeed a better way and founded Ingenious Med to deliver revenue and physician management solutions that help practices be successful to a diversity of healthcare provider organizations.”
At its core, charge capture helps organizations account for the entirety of services they provide patients, which has proven to be a longstanding challenge to healthcare provider organizations. When they go unrecognized by physicians, auditors, and other staff, it’s as though these services were never rendered because they were never billed.
When applied properly with best practices, charge capture not only delivers a demonstrable increase in the number of charges captured, but also a more accurate representation of what has actually occurred. A recently published report of 36 Ingenious Med client ROI studies found that the mean number of charges per patient increased 7 percent.
For a nationally recognized children’s hospital in the Mid-Atlantic, Ingenious Med delivered a $40 million net benefit within three years due to the hospital’s avoidance of penalties and additional Medicare reimbursement. In addition, the client experienced increased workflow efficiency for the billing and coding staff, who no longer had to spend time manually entering charges. These staff were able to refocus on more important tasks that help ensure the hospital gets paid for those charges, such as following up on denials.
While many organizations are feeling the financial pressure mount, Ingenious Med clients are thriving. On which side of the scale do you want to be?
Take the next step and learn more about the impact our clients are seeing in their organizations.
Want to see more? You can find our other blogs here.
Don’t miss out on our next blog! Subscribe here.