Value-based care (VBC) took a backseat during COVID but is poised to be re-energized, according to presenters at our recent webinar. Rohit Uppal, MD, MBA, SFHM, Chief Clinical Officer of Hospitalist Services at TeamHealth and Steven Liu, MD, SFHM, Founder & Chief Medical Officer at Ingenious Med, teamed up to present the state of VBC today and share strategies and tools for revitalizing these programs.
The State of VBC Today
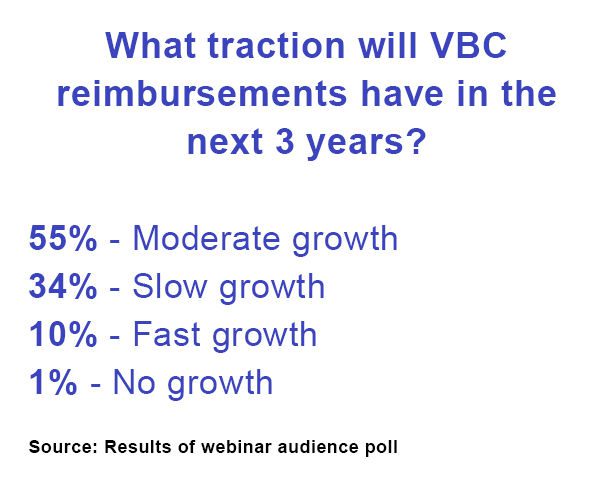
Dr. Liu reported that VBC has continued to experience uneven and sometimes sluggish growth in the U.S. In fact, a recent CHIME survey found that the percent of revenues from fee-for-service (FFS) care actually increased from 74% in 2019 to 76% in 2021 due to COVID. And according to a recent RAND Corporation study, over 80% of compensation for primary care physicians and over 90% for specialists is still volume-based.
While the impact of VBC programs on cost and outcomes has been mixed, Medicare Advantage has demonstrated some meaningful reductions in costs and utilization. This program has grown to serve over 26 million enrollees in 2021 and has saved 9.5% per enrollee and cut avoidable hospitalization for patients with major complex conditions by more than half.
Bundled Payments: An Unclear Future
Dr. Uppal noted that in 2015, TeamHealth was enthusiastic about the first bundled payments program. “Hospital medicine was the perfect specialty to tackle bundled payments. We were already the go-to change agents within hospitals. For years we have worked on improving quality and efficiency within the four walls of the hospital under a bundled payment known as the DRG. Our clinician leaders had to work hard to redesign care and change the physician mindset, but we quickly achieved significant savings under BPCI classic by focusing on quality and outcomes and looking beyond hospital walls.”
 He added, “Classic BPCI placed physicians in the driver’s seat and opened the door to integrating care across silos. Over time there has been a shift; health systems have more often become the initiators of bundled payments and with BPCI-advanced, they have become more selective about which bundles they participate in. At this point, the future of this program is unclear.”
He added, “Classic BPCI placed physicians in the driver’s seat and opened the door to integrating care across silos. Over time there has been a shift; health systems have more often become the initiators of bundled payments and with BPCI-advanced, they have become more selective about which bundles they participate in. At this point, the future of this program is unclear.”
Now that COVID is waning in the U.S., some HCOs are renewing their focus on VBC. Some organizations recognized that over-reliance on FFS reimbursement could be damaging in a pandemic when ED and surgical volumes took a significant hit. COVID also accelerated the shift to lower-cost settings and ramped up efforts to reduce avoidable utilization.
Value-Based Strategies: Start with Physicians
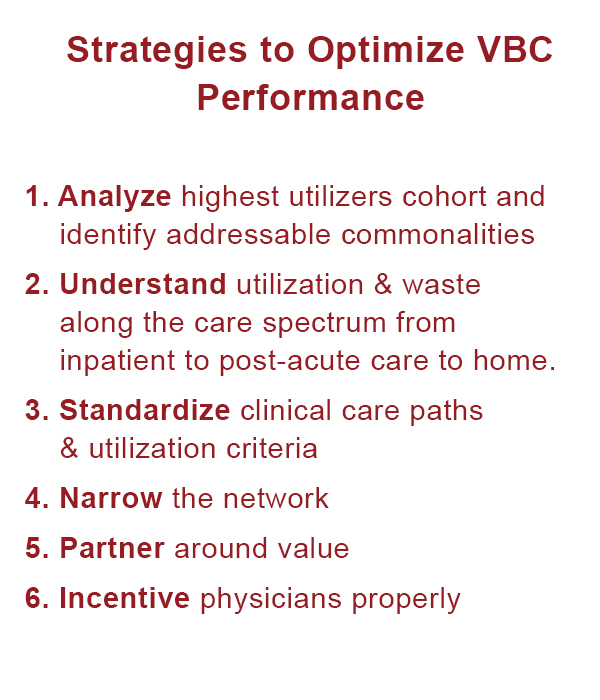
The physicians shared their recommended strategies and tools for increasing VBC performance (also see sidebar).
Engaging and aligning physicians was at the top of the list. “Capturing the hearts and minds of physicians is key, and that means prioritizing what’s in the best interests of patients,” said Dr. Uppal. “Engaging physicians and getting them to see how it’s better for patients drove a change in our culture and mindset that complemented changes in our processes.”
Dr. Liu noted that a recent study found physician-led ACOs saved $218 per patient vs. only $168 for hospital-led ACOs, underscoring the value of physician leadership and engagement.
 Ensuring appropriate physician incentives is also essential. Dr. Liu commented, “incentives should be based on actions that are within physicians’ control. For example, physicians can control when they sign the discharge order, but don’t control when the patient is discharged, so health systems should incentivize them for the time the order is signed.”
Ensuring appropriate physician incentives is also essential. Dr. Liu commented, “incentives should be based on actions that are within physicians’ control. For example, physicians can control when they sign the discharge order, but don’t control when the patient is discharged, so health systems should incentivize them for the time the order is signed.”
Improve Data and Analytics
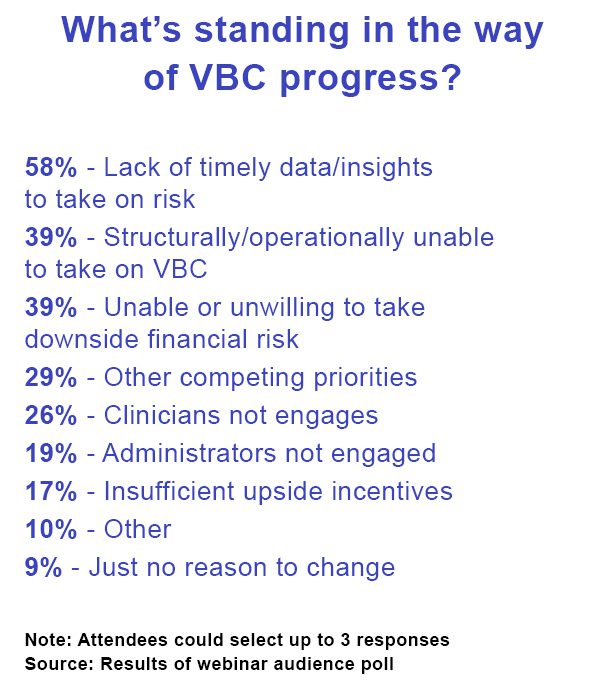
Another critical component of VBC success is ensuring that the HCO has timely, accurate data and insights to monitor productivity, utilization, and outcomes. Yet this remains surprisingly challenging for many organizations; in fact, webinar participants rated the lack of timely data and insights to take on risk as their top barrier to VBC progress (see sidebar).
TeamHealth has used Ingenious Med’s point-of-care solution to overcome the lack of EMR continuity, identify and flag patients, track the next site of care, identify high and low clinician performers, get real-time readmission data, and communicate key clinical information between clinicians. It relies on Ingenious Med to get timely data across all of its locations to ensure it can accurately monitor clinician productivity and appropriately staff each location.
Manage Care Across the Continuum
Dr. Liu stressed that ED visits, admissions, readmissions, and post-acute care still drive a lot of costs. He recommended managing care across transitions and narrowing the network to those who are aligned with your VBC goals. He recommended using technology to analyze the highest utilizers and identify waste along the continuum. Standardizing physician workflows around care paths and admission criteria can also help to deliver more consistent outcomes.
However, our physician presenters advised attendees not to cut length of stay when it risks increasing other utilization. Keeping a patient in the hospital an extra day can save overall costs and improve quality if it avoids skilled nursing facility (SNF) admissions or a hospital readmission.
“Choose the least restrictive next site of care rather than automatically discharging patients to a SNF out of habit or assuming it’s always best for patients.” – Rohit Uppal, MD, MBA, SFHM, Chief Clinical Officer of Hospitalist Services at TeamHealth
Dr. Uppal recommended matching the intensity of services to patients’ needs. “Choose the least restrictive next site of care rather than automatically discharging patients to a SNF out of habit or assuming it’s always best for patients.”
When a SNF is the right option for a patient, focus on reducing LOS and readmissions by creating SNF performance networks that partner on quality and cost of care; build a foundation for clinician collaboration through data, meetings, and other support; and track and share performance data by facility.
Dr. Uppal said, “We have SNFists who help manage LOS and quality in the SNF. Their daily presence and responsiveness helps prevent unnecessary ED visits and admissions. By creating connections between the SNF clinician and ED physician, we can avoid unnecessary admissions even for those patients that need an ED evaluation. So, that patient who just needs a CT scan can get the test they need and then return to the SNF instead of having an unnecessary hospital admission.”
Also use telemedicine. The increased use of this technology was a silver lining of the pandemic, according to Dr. Uppal. “Early on, we utilized telemedicine to protect our clinicians from exposure and illness. Later we used telemedicine to provide additional capacity to address local surges. We also have learned to monitor stable but at risk patients by using remote patient monitoring to conserve inpatient resources for the acutely ill. We are using ED follow-up telemedicine visits to allow ED physicians to safely transition patients home who might otherwise require observation.”
Dr. Liu noted that the hospital at home model is another approach that has been shown to provide cost-effective care with equivalent health outcomes.
The presenters made clear that, in any payment model, physician engagement, good data and analytics, good communication and care coordination, and the right payment incentives are a recipe for success.