by Steven Liu, MD, SFHM, Founder and Chief Medical Officer
Our recent webinar, Overcoming Blind Spots: Using Analytics to Improve Performance, examined the challenges that healthcare executives face in getting actionable insights. I had the pleasure of speaking with a fellow physician and administrator, Gerald Groff, MD, Chief Medical Insurance and Innovation Officer at Bassett Healthcare Network. We also asked over 100 participants about the barriers they face in optimizing revenues.
Dr. Groff reminded me what an amazingly hard task it is to align physician and hospital performance and achieve interoperability across the care continuum. While Bassett has been evolving their EHR system for some 20 years, they still consider their ability to turn data into insights and to align physician performance a work in progress.
The power of the physician keyboard and physician alignment
The physician’s keyboard is one of the most powerful tools in healthcare. Health systems are more likely to succeed when they can engage them and align goals. But physicians are drowning in data tasks, resulting in less time for patient care and unprecedented rates of burnout. We have to avoid asking them to do one more task or make extra clicks. We must also get better at sharing meaningful data to arm them with information they need, when they need it.
That requires using additional tools to analyze physician performance at the individual physician level as well as the practice level. As a practicing physician, I know that we tend to be competitive and will change behavior when we have comparative data that is trustworthy, timely and meaningful. At the same time, I appreciate how difficult that is.

Even a health system like Bassett, which employs hundreds of providers and has a single EHR, and has internal RVU benchmarks, faces tremendous hurdles. A solution like Ingenious Med – which is based on claims data that physicians have entered themselves – enables health systems to deliver credible and timely insights to benchmark their performance.
Bassett tackles a few priority projects at a time to allow physicians to absorb and react to the findings before moving to the next project. They also share data with physicians, invite them to find any flaws, and then fix issues when needed. They recognize that you have to expect, and even invite, physicians to nitpick the data.
Poll results: Top barrier to optimal revenue capture is physician alignment
The results of a poll we conducted during the webinar were consistent with the experience of Bassett and our customers. Participants reported that their top barriers to optimizing revenue capture were aligning physicians and organizational goals (45 percent), followed by missing data and insights (38 percent).
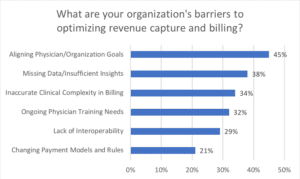
N = 56
Source: Ingenious Med webinar, September 18, 2019, “Overcoming Blind Spots: Using Analytics to Improve Performance”
Optimizing revenue remains critical during IT conversions under any payment model
Despite (or perhaps because of) the rise of value-based care, revenue cycle management has never been more important. Thin margins make it critical to capture all revenue earned. And even in fee-for-service care, health systems need to know how their true care costs compare to the reimbursement for that care. Even large integrated providers like Kaiser use Ingenious Med for accurate claims capture, which continues to be a critical part of their business.
Dr. Groff noted that Bassett experienced a significant reimbursement delay when they installed their EHR’s revenue cycle software that required a months-long correction process. They also uncovered previously unknown problems – including that providers weren’t fully capturing all diagnoses in their most-acute patients and that the constant onslaught of payers’ rule changes made it difficult to keep providers up to date.

That’s where an automated solution can come to the rescue. Our mobile platform makes it easy for providers to capture complex charges at the point of care – ones that an EHR would typically miss – and for health systems to continue to monitor and optimize productivity.
Payment models aren’t binary
People often speak about fee-for-service and value-based care as if they’re binary, but I see them along a spectrum that moves gradually from zero to full risk. Dr. Groff noted they’ve had great success on a project-by-project basis, but that it’s hard to have an impact on the population as a whole without a fully capitated environment. They’re gaining experience with their own self-insured employee health plan to test their analytics there, then apply what they’ve learned to other value-based models.
Agnostic solutions help bridge care continuum gaps
Despite receiving some data from the State of New York’s data repository and employing a large cadre of physicians, Dr. Groff noted that Bassett remains challenged to gather data from outside their health system. Even using their EHR’s community connection tool merely enables their non-employed providers to do a passive data lookup rather than permitting true interoperability.

That problem also exists in the post-acute world, where skilled nursing and other post-acute providers typically use different EHR platforms and may even be paper-based. And patient navigators and others in the home care field are typically on different EHR platforms; getting data across both ends of the care continuum remains challenging without a third-party solution like ours that is agnostic and that can bridge the gaps.
That’s why it’s so critical to look beyond your EHR for purpose-built solutions that can make data interoperable and bridge communication gaps between care settings. It’s the only way to get a more holistic picture of patients, provide more coordinated care and ensure that you’re adequately compensated for the care you deliver.
Want to see more? You can find our other blogs here.