Success in value-based care requires aligning physician performance with Triple Aim goals: reducing per capita healthcare costs, increasing care quality and improving population health. We monitor quality measures and metrics that enable you to reduce costs, manage utilization and enable appropriate transitions across the healthcare continuum.
Value-based rounding
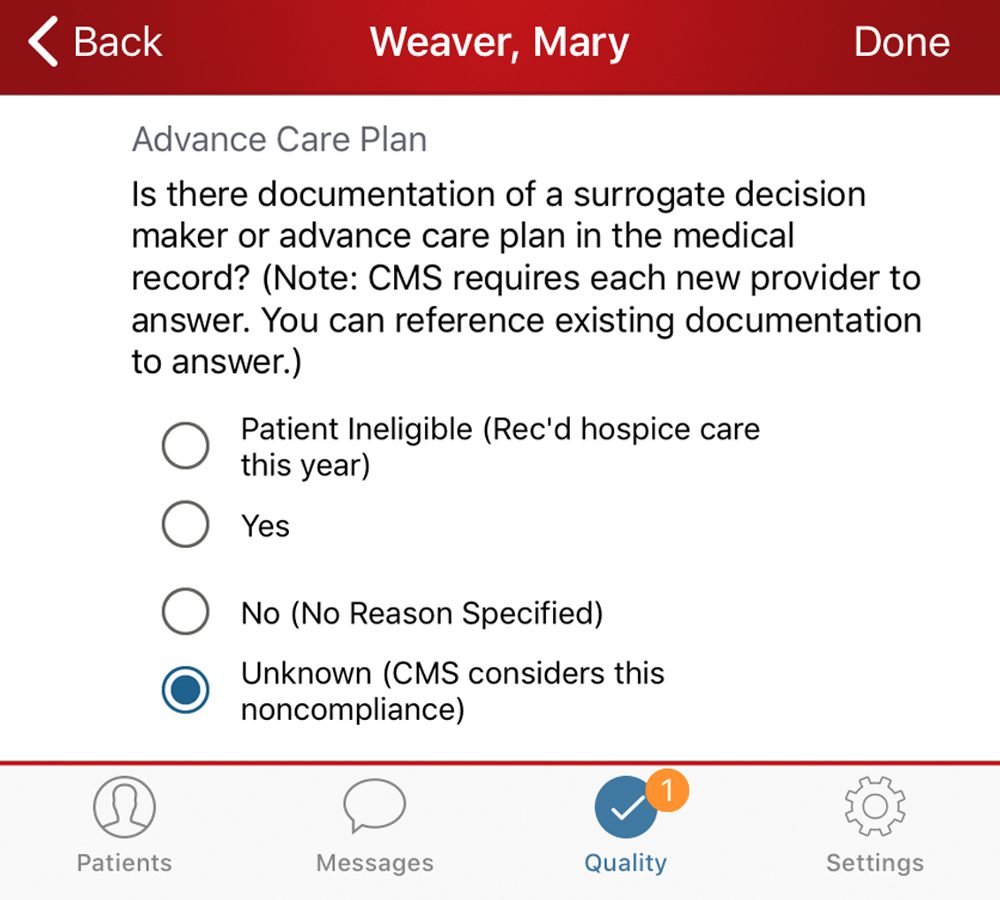
Align physicians with value-based goals and requirements as they round by accurately tracking quality metrics.
- Automatically identify and track members of value-based programs (BPCI, ACOs, case rate and more) and/or high-cost patients.
- Align providers on management of costs and care transitions.
- Reduce unnecessary bed days and avoid readmissions.
Enhanced care team collaboration
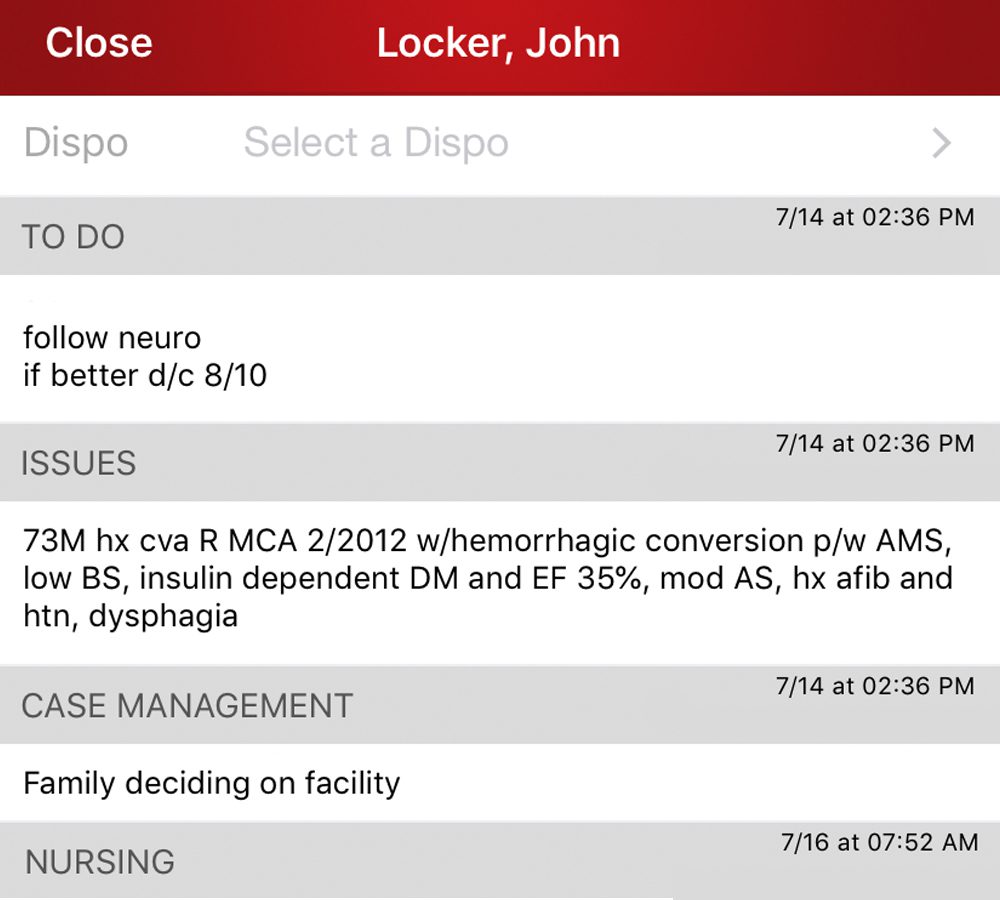
Improve communication and coordination across the organization with tools that facilitate provider collaboration regardless of location, service or device.
- Ensure continuity of care with HIPAA-secure notes and messaging.
- Enable virtual huddles to quickly share patient information, disposition logistics and more across care teams.
- Connect administrators and back-office staff directly to front-line providers.
More efficient patient throughput
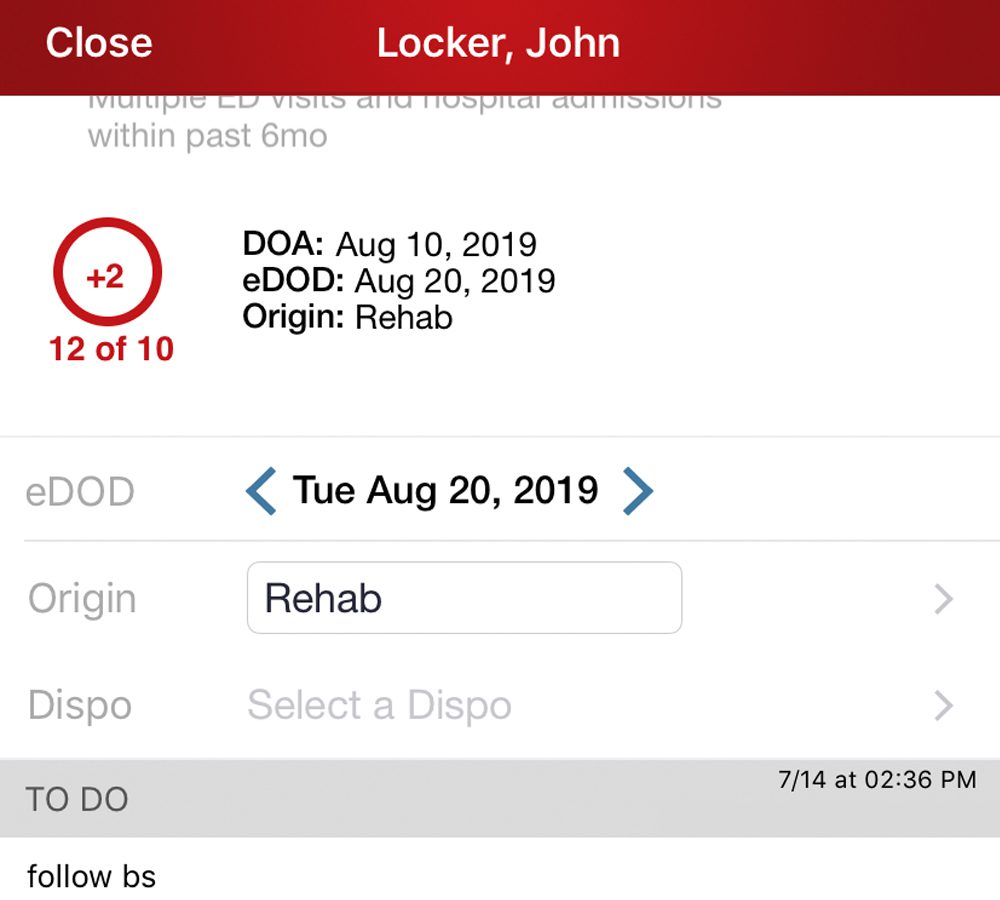
Track anticipated discharges to ensure efficient throughput across healthcare settings and minimize costly avoidable bed days.
- Proactively manage discharge barriers and coordinate care transitions.
- Highlight estimated discharge dates for patients in value-based programs.
- Reduce unnecessary length of stay where appropriate.
Intelligent care transitions
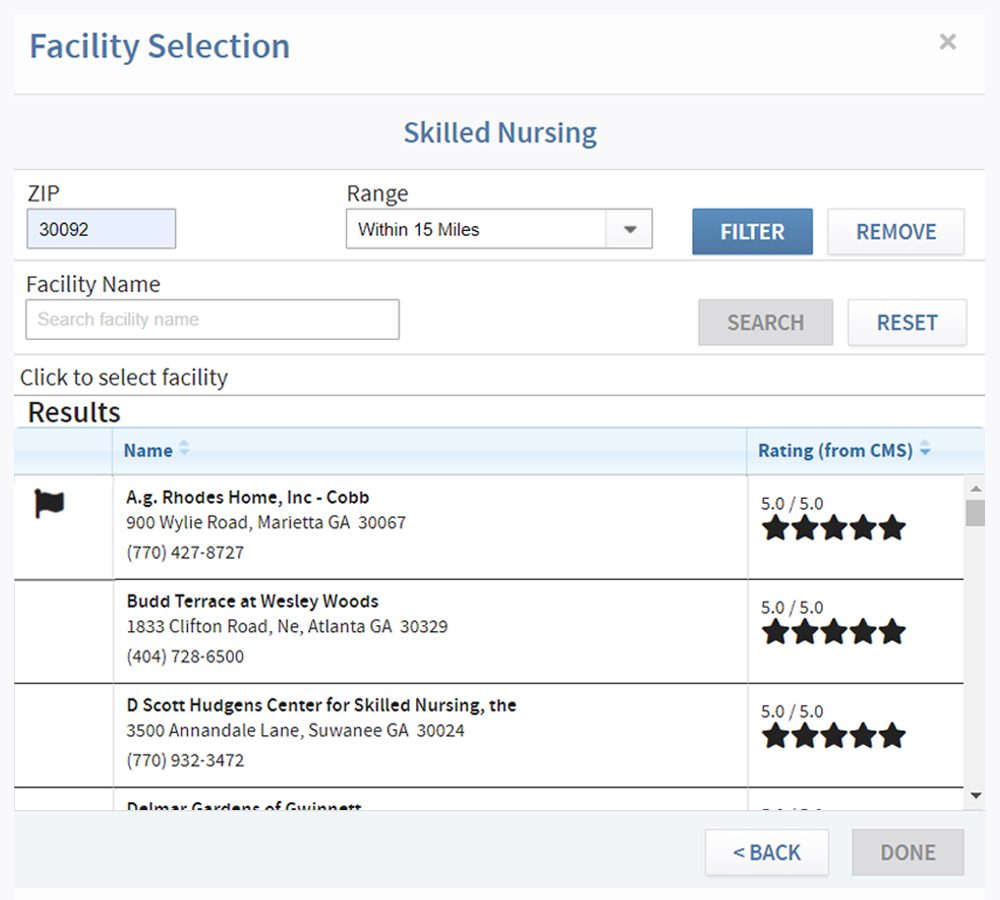
Automatically identify and manage bundled care patients and ensure appropriate care transitions to the correct locations and preferred network facilities.
- Automatically identify and track BPCI patients.
- Easily select the lowest-cost, highest quality post-acute disposition settings.
- Ensure patients stay within preferred network providers.