Heading into the New Year, healthcare provider organizations are now actively investing in AI to address persistent revenue cycle management (RCM) obstacles, according to independent research funded by Ingenious Med.
Why? The research reveals that leaders who are investing in AI are anticipating that the new technologies will not only help their organization overcome ongoing revenue cycle challenges but also contribute to driving significant revenue growth.
Survey Snapshot: Unsatisfactory RCM Tools, Unmet KPIs
The results show that the top revenue cycle management challenges include claims denials, underpayments, accounts receivable (A/R) management, and charge capture, among others.
Further, participating executives indicate that the revenue cycle management solutions their organization have in place today are largely unsatisfactory and, equally important, not effective at meeting business goals aligned with key performance indicators (KPIs).

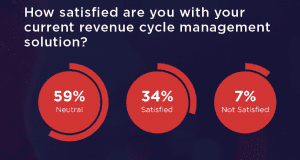 Only one third (34%) of survey respondents are “satisfied” with their current RCM solutions, in fact, and fewer (30%) say their revenue cycle tools perform “very well” when it comes to helping their organization achieve financial KPIs. The top challenges respondents face with their current RCM solutions include general inefficiency, missing charges, charge lag, and coding errors.
Only one third (34%) of survey respondents are “satisfied” with their current RCM solutions, in fact, and fewer (30%) say their revenue cycle tools perform “very well” when it comes to helping their organization achieve financial KPIs. The top challenges respondents face with their current RCM solutions include general inefficiency, missing charges, charge lag, and coding errors.
Considering that survey respondents rank their top KPIs as net A/R days, denial write-offs, denial rates, cash on hand, revenue recognition/charge lag, and individual physician performance, a correlated and concerning finding is that organizations are failing to collect 11.4% of reimbursements every year. That degree of revenue leakage would be problematic for any business, and health systems, hospitals, and practices already operating on tight margins are no exception.
How AI Can Address Pressing RCM Problems
The research shows that executives are looking for new tools to improve revenue cycle performance, including AI, automation, and smart analytics.
At least 90% of participating executives indicate AI can perform well at managing patient payment estimations (97%), payment amount estimations (96%), coding (94%), charge capture (94%), cash flow (91%), and payer payments (90%) — while 88% and 86% say the same about denials management and patient payments, respectively.
Executives indicate that their preferred method for incorporating AI into RCM processes is via a revenue cycle vendor, followed by a practice management vendor, and then leveraging internal IT resources to build their own. The fewest percentage of participants work with a consultant to create a custom AI solution.
Additionally, 78% of leaders would like to have smart analytics for identifying instances of undercoding and overcoding, and to improve charge capture with their revenue cycle solutions. That interest stems from the 13.3% of charges being under-coded and 7.4% that are over-coded, both of which can lead to claims denials, payment delays, and lost revenue.
While participating leaders say they are investing in AI for RCM within the next 1-3 years, the survey findings indicate that leaders are also looking to AI to achieve greater efficiencies, better financial performance, fewer denials, a leaner workforce, and more accurate coding.
Executives’ Expectations for AI: Fueling Strong Revenue Growth
 Leaders have high expectations that implementing AI, automation, and smart analytics will yield double-digit revenue increases in a number of areas. Survey respondents anticipate the tools will drive approximately 20% increases in revenue when it comes to some of their organization’s KPIs, including: payer amount and payments, coding, claims lifecycle, patient payments, and denials prevention and management.
Leaders have high expectations that implementing AI, automation, and smart analytics will yield double-digit revenue increases in a number of areas. Survey respondents anticipate the tools will drive approximately 20% increases in revenue when it comes to some of their organization’s KPIs, including: payer amount and payments, coding, claims lifecycle, patient payments, and denials prevention and management.
Ultimately, the research illustrates that health system, hospital, and medical group leaders are investing in AI to bolster their organization’s bottom line by fortifying RCM processes: 82% of respondents say AI will have a positive impact on their revenue cycle, and 73% believe AI will be widespread in revenue cycles within five years — a notable increase from the 60% who said that in 2023.
Ingenious Med commissioned Sage Growth Partners to independently recruit and survey 101 finance and operations leaders representing health systems, independent hospitals, physician practices, and ambulatory surgery centers. All research was double-blinded and participants were screened to ensure familiarity with their organization’s RCM processes and solutions.
To learn more about healthcare leaders investment plans and expectations when it comes to AI in the revenue cycle, download the full report, From AI Optimism to Action: Where Health Systems, Hospitals, and Practices are Investing Now to Fortify Revenue Cycle Management.