Rising to the Challenge: How Leading Healthcare Organizations are Thriving in an Evolving Revenue Environment

Lower volumes, changing case and payer mixes paired with greater uncertainty about positive operating margins make revenue optimization more essential than ever for healthcare organizations. But what are the best approaches in healthcare reimbursement for thriving in today’s uncertain financial environment?
We’ve asked leaders from several physician management organizations and healthcare systems to share their strategies for overcoming the considerable challenges of this altered landscape. They describe how they used data and analytics to better manage capacity, coordinate care, optimize revenues and adapt to changing reimbursement.
The Pandemic Has Made Managing Healthcare Finances Even Harder
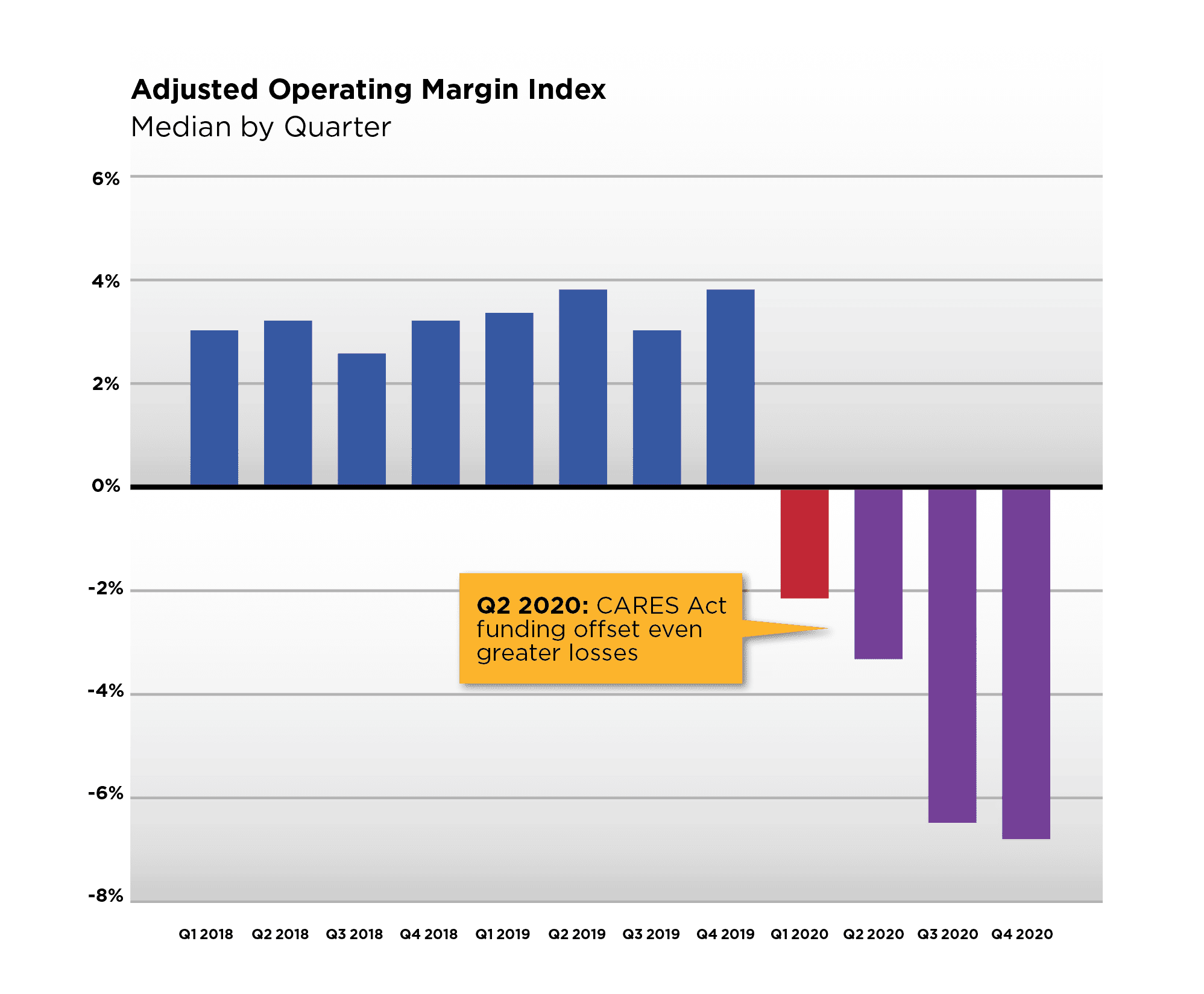
Operating health systems and physician practices has always been hard, but the COVID-19 pandemic has created new challenges to profitability in 2020 despite significant federal subsidies. Before the pandemic, healthcare financial cushions were already thin. In 2018, health system operating margins were 30% lower than 2015 levels.[1] And Kaufman Hall found that more than 30% of U.S hospitals had negative margins in 2019.[2] (See Figure 1.)
COVID-19 only made it harder to operate in the black. A July 2020 HFMA survey of 174 healthcare leaders found that 89% of respondents expect 2020 revenues to be lower than pre-pandemic levels, and 62% project that those losses will be 15% or greater.[3]
Hospitals and physician practices have both experienced financial pain. During the spring of 2020, hospitals lost $60B per month as surgical volumes declined by 61%, discharges by 30%, and ED visits by 43%.[4] While volumes are rebounding, an American Hospital Association (AHA) report projects that hospital financial losses will deepen by an additional $120.5 billion in the second half of 2020, bringing total losses to at least $323.1 billion for the year.[5]
Figure 1.
The AHA report states, “Experts have warned that the recovery pace for hospitals and health systems will be slow and that normal hospital volume will not come back quickly even as states lift moratoriums on non-emergent procedures.”
On the physician side, the picture was also bleak. In April 2020, physician practices shed 243,000 jobs[6] and lost an average of 55% of their revenues.[7] As a result, 53% of physicians reported feeling very or extremely concerned about the pandemic’s long-term impact on their practice.[8] Data from the Ingenious Med® application show that this concern may still be warranted. Billings dropped a massive 40% by April 2020. After rebounding in July and trending back up to 90% of pre-COVID levels by August 2020, bills created per day dropped off again to around 75% of typical volumes in September 2020.
Effective Strategies for Optimizing Revenues and Resources
How have leading healthcare entities risen above COVID-19’s myriad challenges to maximize productivity, cope with dramatic volume and casemix changes, and optimize revenues? Using examples from American Physician Partners (APP), US Acute Care Solutions (USACS) and a major medical group at a southwestern health system, we asked healthcare leaders to share the strategies that have enabled them to succeed in an evolving revenue environment. Their ideas for optimizing the revenue cycle focused on using data and analytics to manage capacity, coordinate care, optimize resources and adapt to changing reimbursement models.
1. Manage Demand by Tracking Real-Time COVID-19 Volumes
Having accurate and timely data is critical to success. Key data includes census data and real-time COVID-19 patient volumes that can be viewed across the organization at all locations. Sharing data from these sources enabled these organizations to gain insights into volume fluctuations that have been helping them right-size their resources during the pandemic.
Dennis Deruelle, MD, FHM, APP’s Executive Director of Hospital Medicine, noted, “After seeing a roughly 45% drop in ER volumes and a 35% drop in hospital medicine volumes this spring, we had to make rapid staffing changes to match the lower demand. Fortunately, we use a staffing grid developed internally plus performance dashboards that include encounters per day and total encounters to calculate our productivity. We could review our census on a daily basis for every practice, and track the trends to help us project the upcoming week. That allowed us to identify hotspots and shift resources accordingly.”
After rebounding in July and trending back up to 90% of pre-COVID levels by August 2020, bills created per day dropped off again to around 75% of typical volumes in September 2020.
USACS also used analytics to adapt its budget and staffing as patient volumes fluctuated during the pandemic. An administrative dashboard proved helpful for spotting spikes in census, LOS, readmissions and more. It enabled administrators to focus additional resources on sites that were receiving an influx of COVID-19 patients.
Leaders at APP, USACS and the southwestern health system took advantage of new automated COVID-19 identifiers and trackers developed by Ingenious Med to check COVID-19 patient volumes multiple times a day. Clinicians at each site used this real-time data to spot potential capacity issues due to physician staffing availability and allocate resources accordingly to support their sites while minimizing waste. Having daily census data also enabled their physicians to better plan their daily schedules.
“We could review our census on a daily basis for every practice, and track the trends to help us project the upcoming week. That allowed us to identify hotspots and shift resources accordingly.”
Dennis Deruelle, MD, FHM, Executive Director of Hospital Medicine at APP
Andrea Funk, VP Integrated Acute Care Operations at USACS, also found this data helped identify areas where it needed to deploy its telemedicine backup plans in case providers got sick and were unable to work onsite. “Having Ingenious Med helped us stay focused during this crisis,” she explained. “The platform made it much easier to reassign physicians from less busy areas – like the emergency department and anesthesiology – to help staff our critical care areas, where we greatly needed the help.”
APP used telehealth as a backup for managing overflows. “When you cut staff, hospitalists worry that there could be days when they get overwhelmed, even though that rarely happens,” stated Dr. Deruelle. “So, we put virtual visits in place to manage any overflow, which was invaluable in reducing physician concerns.”
2. Plan for a Potentially Longer Length of Stay
The unique aspects of COVID-19 meant that all three organizations had to prepare for a much longer LOS for patients with the virus. Funk said, “Managing co-morbidities was critical to managing LOS in COVID-19 patients. In contrast to our average LOS of 3.8 days, their average LOS was closer to 20 days and sometimes lasted over 100 days. Even when COVID-19 patients are stable, we often can’t discharge them to long-term care because they’re still on CPAP [continuous positive airway pressure devices]. That keeps them stuck in the hospital and creates back-ups.”
USACS used its COVID-19 dashboard to receive an accurate daily update of these patients by location, which enabled administrators to anticipate which facilities would need to get temporary privileges for a pool of physicians and APPs who were helping to manage the surge. The southwestern health system used the platform’s analytics dashboard to help practices track the higher LOS for COVID-19 patients and the much lower census. Two key measures, LOS and readmission rates, flow from the Ingenious Med app into that scorecard, enabling medical directors at each site to drill down by physician to see which ones needed help managing LOS.
3. Use Analytics to Manage Productivity and Modify Physician Incentive Compensation
APP and the southwestern health system found that being able to use indicators to identify COVID-19 patients also helped to manage productivity without overburdening their physicians. Since these patients consumed more physician time, administrators could determine when to reduce the number of patients assigned to a hospitalist.
“We were able to track productivity by patients per shift and see whether we were ‘green,’ which meant we were at 100% productivity.”
Dennis Deruelle, MD, FHM, Executive Director of Hospital Medicine at APP
The southwestern health system’s medical group had to cancel all elective surgeries in March, contributing to a loss of about 50% of volumes and over $620 million in revenue. It sought to avoid layoffs by developing different staffing structures, offering voluntary severance packages and reducing hours and schedules.
The group used Ingenious Med data to adjust its productivity targets and to enable physicians to easily track their performance against the new compensation targets.
Derick Perkins, Managing Partner of Metis Advisors, LLC, worked extensively with this health system’s medical group. “Over-communicating to physicians and clinical staff was critical,” he said. “Doctors were upset because they know volume losses impact their RVUs. Reassuring them that their compensation targets would be adjusted helped to allay concerns.” When volumes began rebounding to about 70% of normal in July and August, the group could modify staffing and targets accordingly.
Dr. Deruelle noted that APP used its analytics dashboard to track the hours cut as well as total hours. “We were able to track productivity by patients per shift and see whether we were ‘green,’ which meant we were at 100% productivity. We could view our productivity by site every single day. That was extremely helpful because then we could tell our site medical directors, ‘This is the staffing that we want, and this is what you’re shooting for.’”
As part of its provider engagement efforts, Adfinitas provides coding education to its physicians and advanced practice providers and requires them to monitor their performance using Ingenious Med’s reports. “It’s very easy for them to do and they can get reports in just a few minutes,” said Dr. Mitchell.
4. Capture Charges Efficiently and Accurately at the Point of Care
To optimize revenues, Perkins recommended going back to basics while taking advantage of efficient technology. Prior to the pandemic, the southwestern health system was well-positioned to capture charges because it had switched from highly inefficient manual revenue cycle processes to using both Ingenious Med and its EHR system, Athena Health, to capture all charges efficiently.
“The health system leveraged the power of both systems to identify the most appropriate codes,” Perkins explained. “It helped reduce charge lags and got claims out the door faster, so we could get paid quickly and correctly.”
“Before the new system, inpatient physicians had charge lags as long as 30 days. Afterwards, charge lag went down to six days as a result of capturing charges accurately at the point of care.”
Derick Perkins, Managing Partner of Metis Advisors, LLC
He added, “Before the new system, inpatient physicians had charge lags as long as 30 days. Afterwards, charge lag went down to six days as a result of capturing charges accurately at the point of care.” The health system’s medical group used the Ingenious Med MasterCoder tool to help improve coding speed, accuracy and compliance while reducing coder workload and the amount of coding staff required. It also reduced the number of denials resulting from filing claims late.
5. Educate and Support Physician Charge Capture
The pandemic has made it more essential than ever for hospitals and physician practices to collect all the revenue to which they are entitled while minimizing the cost to collect.
Coding accurately is an important step in avoiding undercoding and lost revenue while improving the allocation of back-officeresources and using them more efficiently – both important actions given today’s tighter margins.
The southwestern health system also invested heavily in ongoing physician education to help avoid undercoding and overcoding at the point of care. Instead of performing charge entry, coders could focus instead on reviewing and reconciling charges to increase compliance. The platform enables quality assurance staffto pull the missing bills report from the system (as well as other reports) to monitor each practice and identify any missing charges.
APP used a similar approach. “We believe that the physician should pick the code, not a coder,” said Dr. Deruelle. “We use coders to provide oversight or make suggestions to ensure documentation and coding are accurate, but physicians deliver the care and they know exactly what services were provided.”
USACS used the tool to stay current with each site’s activity from a practice management standpoint. “Our physicians were amazing, and we pride ourselves on them capturing their charges the same day or in real time,” Funk explained. It also used the platform to quickly create superbills for staff temporarily assigned to care for COVID-19 inpatients, such as emergency medicine physicians who weren’t used to submitting their own charges.
The value of a dedicated physician charge capture and practice analytics solution
Having a dedicated physician charge capture and practice analytics platform focused specifically on your practice’s needs and goals can be the key to success in this environment where managing scarce resources, controlling productivity and billing for every service rendered is essential for survival.
Healthcare organizations must be able to evaluate and standardize performance between individual providers as well as across teams and practices. They also need to deliver timely, actionable insights to the front-line clinicians who directly affect productivity, performance and revenues.
Doing so relies on capturing revenues accurately at the point of care. Real-time data enables clinicians and administrators to identify issues and spot trends, as well as underlying causes. When an intuitive interface that can deliver insights without impacting workflows is combined with a mobile, point-of-care application, organizations can extend practice analytics to all stages of the patient.
6. Reduce Denials by Holding Claims to the Point of Discharge
The southwestern health system learned an important lesson along the way. It was initially reluctant to hold claims until the time of discharge, and instead continued releasing claims as soon as they were received in the practice management system. The health system eventually switched when it realized that holding claims to clear inside the platform helped to catch certain issues and avoid duplicate charges.
7. Create Payer Report Cards
To ensure that payers are reimbursing at the contracted rate or at the advertised telemedicine rate when the pandemic first hit, Perkins recommended keeping a report card for major payers to track this data. He stated, “For example, we found that some payers are not reimbursing for telehealth as much as they had promised, so I truly believe every organization should have a payer report card. At a minimum, that report card should track how much you’re collecting versus your contracted rate as well as your denial rate with that particular payer.”
“You need to hold payers accountable.”
Derick Perkins, Managing Partner of Metis Advisors, LLC
Perkins added, “The need for payer report cards pre-dates COVID-19, but the pandemic has made it essential to go back to the basics and make sure you’re getting paid according to your contract. You need to hold payers accountable. You could consider partnering with an underpayment firm on a contingency basis, and make sure you regularly update your fee schedules and track denials closely. We found that payers may say their systems are ready to take certain codes, but then deny them. This causes more work for collectors and ultimately increases A/R Days.”
8. Develop a Comprehensive Self-Pay Strategy
The pandemic dramatically swelled the ranks of the unemployed and accelerated the trend of patients paying for more care out of their own pockets. Continuing a practice it had started before COVID-19 hit, the health system’s medical group developed a comprehensive self-pay strategy that included offering patients financing options through a medical credit card company.
Perkins noted, “COVID has increased the percent of self-pay patients and patients today have higher out-of-pocket responsibilities than they used to. Several government programs have provided some relief for self-pay balances, enabling health systems to file those claims to this program and receive reimbursement if they meet certain criteria.” He also noted that organizations can provide patients with other options, such as internal payment plans including working with patient financing firms for extended payment options.
9. Make More Informed Bundled Payment Decisions
APP and many of its hospital partners participate in value-based models such as bundled payment programs. Dr. Deruelle commented, “CMS has given bundled payment programs a reprieve, so we could just push this year if we want to avoid losing money. Or we have the option of pulling every COVID patient out. Thankfully, our platform allows us to identify all our COVID patients and pull them out of the model if we wish, so we can determine which is the ideal option for our organization.”
10. Improve Throughput Across the Continuum
The highly infectious nature of COVID-19 meant that fewer patients could be discharged to skilled nursing facilities. The Ingenious Med platform’s COVID-19 identifiers proved useful in helping organizations proactively identify infectious patients so they could better plan for discharges and improve coordination with case management departments. That, in turn, helped reduce bottlenecks elsewhere in the hospital and improve throughput.
“The reports enabled us to quickly improve communication, discharge patients timely and decongest emergency departments that needed it.”
Andrea Funk, VP Integrated Acute Care Operations at USACS
Funk explained, “We used the anticipated discharge flag identifier to send a daily report to our site hospital case managers so they knew in real time each day who was going home. We found that some hospitals had perhaps 20 patients in the emergency department that needed inpatient care but were boarded in the ED because no inpatient beds were available. The reports enabled us to quickly improve communication, discharge patients timely and decongest emergency departments that needed it.”
Another strategy that proved effective for USACS was partnering with one of its hospital systems and state officials to open a specific treatment facility to care for infected patients. “When the skilled nursing facilities couldn’t admit new COVID-19 patients or take their own patients back, we deployed a team of providers to expand an empty facility to care for COVID patients exclusively, which took pressure off the other hospital system inpatient units and relieved local emergency department backups,” Funk observed.
Lessons Learned
When the healthcare world is turned upside down by a pandemic – and when collecting every dollar has never been more critical – organizations with point-of-care charge capture tools and accurate, real-time analytics will be better positioned to weather the crisis than those that lack insights and are flying blind.
Predictions about what the coming year holds for healthcare organizations in terms of volumes, revenues, casemix and payer mix vary widely. Having the right tools to manage capacity, optimize revenues, adapt to changing casemix and reimbursement, and coordinate care across the continuum, will help organizations to more accurately predict and more nimbly respond to that future.
While it’s ideal to have these tools in place before a crisis, it’s never too late to get started. Mobile tools that deliver cutting-edge analytics based on timely and accurate data that physicians themselves can enter at the point of care make monitoring key metrics such as LOS and productivity far easier for clinicians and administrators alike. When such solutions can be easily integrated with existing EHRs and IT systems and when they are designed to be intuitive for physicians to use, organizations can quickly get up and running before the next crisis hits.
For more information about Ingenious Med or to request a free demo, call 770.799.0909 or visit online at ingeniousmed.com.
About Our Contributors
Dennis Deruelle MD, FHM, is Executive Director of Hospital Medicine with American Physician Partners (APP) in Nashville, TN. He supports the management of APP’s hospital medicine program and provides clinical oversight to its hospital medicine physicians and advanced practice clinicians in support of the company’s ongoing quality efforts. Dr. Deruelle has over 15 years of hospital medicine leadership experience, having served as the owner of a private hospital medicine practice and CEO/Founder of a boutique healthcare consulting company.
Andrea Funk, RN, MEd, CPHQ is Vice President of Integrated Acute Care Operations at US Acute Care Solutions. She applies her more than 20 years’ experience in nursing, quality management and patient safety to supporting hospital administration, physicians and staff in their daily practice and quality improvement initiatives. Ms. Funk provides expertise in site practice operations, including improving quality metrics, through her commitment to the professional development and support of all clinical and operational staff.
Derick D. Perkins is a Revenue Cycle Leader with over 23 years of experience working with large health systems across the country. He has performed successful revenue cycle optimization projects at Ascension Healthcare, Allina Health, LifePoint, Christus Health and oversaw the unprecedented growth of the Memorial Hermann Medical Group from less than 200 providers to over 800 providers. Mr. Perkins is the founder of Metis Advisors LLC, a consultancy that improves the financial health of rural and smaller practices through revenue cycle optimization and recovery.
Sources: